Post by Sai Kiersarsky, NW Noggin volunteer and Portland State University teaching assistant for the Advanced Neurophysiological Psychology course (Winter term 2019)

Sai joined fellow NW Noggin volunteers, along with students and teachers from Fort Vancouver High School last week to attend Providence Brain Watch, an innovative educational outreach program that introduces young people to healthcare careers – and neuroscience – by inviting them to watch a brain surgery! Here is Sai’s description of his day in the hospital…

Sai in San Diego Public Schools during the 2018 Society for Neuroscience conference
LEARN MORE: Synapsing in San Diego @ SfN!
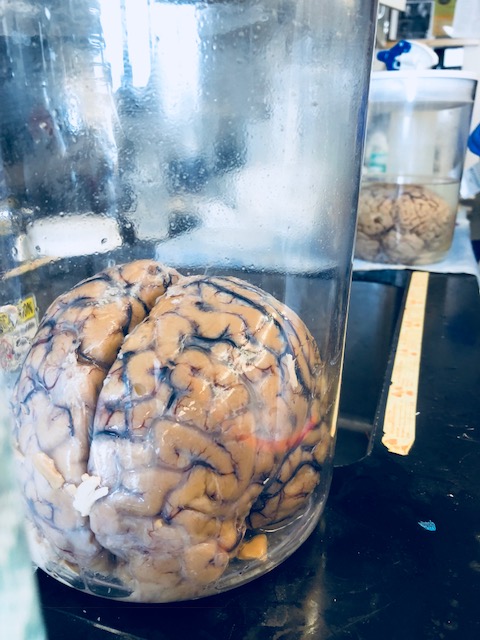
What is it like to witness a brain surgery? The brain is something we are all familiar with to some degree, but we’re familiar with it in a somewhat unfamiliar way. We see diagrams and pictures of it, read articles about it, and if one attends Northwest Noggin events, one can actually hold a real human brain, but rare is the sight of a living brain.

Paradoxically, the brain is the thing we are most familiar with in the entire universe – everything we experience including the experience of you reading this right now is happening in your brain. There is no knowledge that is more direct than the knowledge of your direct experience, happening right now, generated by your brain. Yet, despite this familiarity, the brain is mysteriously alien and elusive, in most cases perpetually locked in the darkness of the skull, forever hidden, yet it’s always right behind the eyes of everyone you interact with.

The chance to peer through that protective skull and actually see a living brain is uncanny – somewhat unsettling and utterly fascinating. Thanks to Providence St. Vincent Hospital, the Oregon Clinic, and Northwest Noggin, students were able to witness this dramatic and high-stakes story as it unfolded right before our eyes.
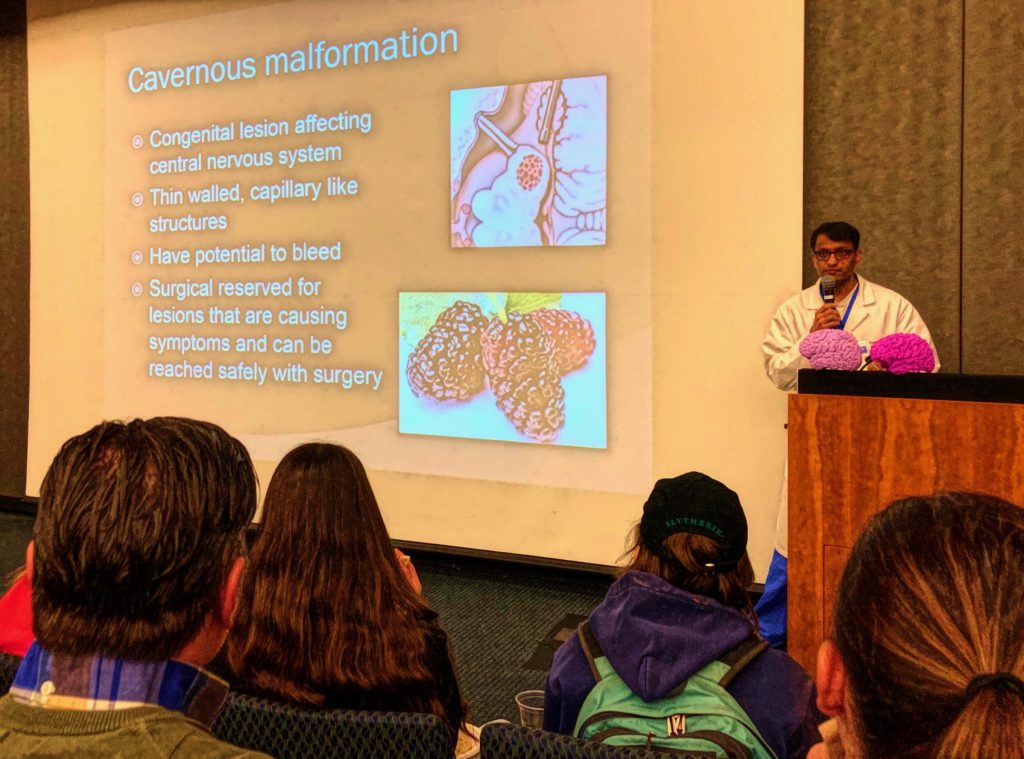
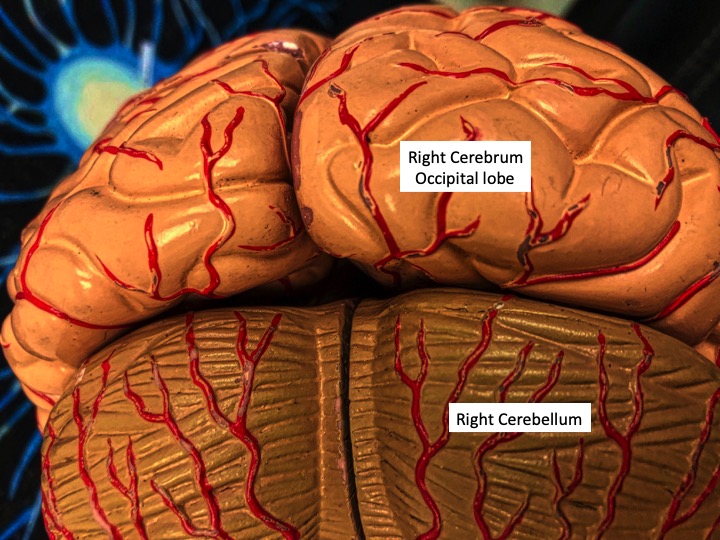
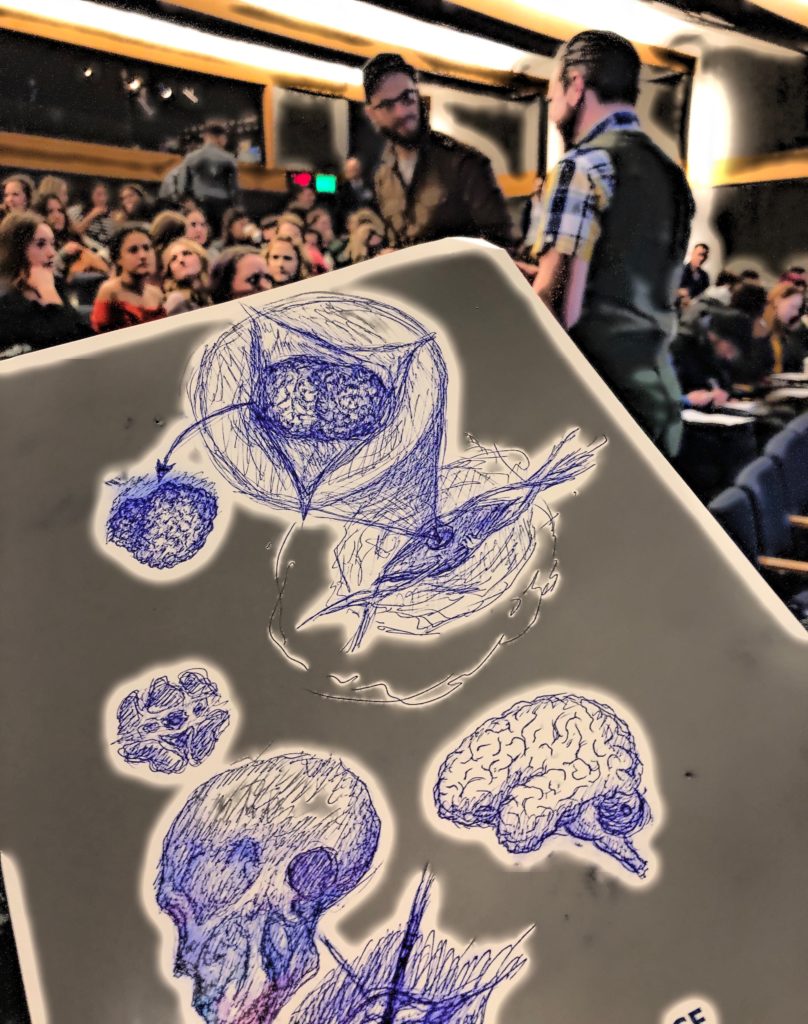
At this event called “Brain Watch,” students gathered in a surgical auditorium to witness Dr. Vivek Deshmukh, a cool and calmly charismatic vascular neurosurgeon, remove a 2.4 cm cerebral cavernous malformation from a patient’s right cerebellum. The entire operation was captivating and vivid, with many varying stages. To the fascinated eyes, ears and brains of the audience, Dr. Deshmukh and a surgical assistant calmly explained his techniques and why he was performing them throughout the duration of the procedure. Their explanations of the surgery were so accessible that every action was so clear; in fact, as the saying goes, it wasn’t brain surgery. But, it wasbrain surgery. And there we were!
LEARN MORE: Cerebral Cavernous Malformation Information Page
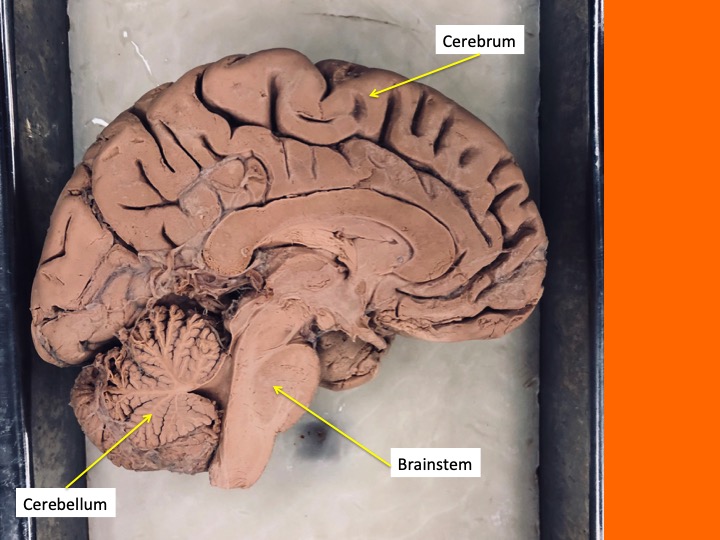
When we encountered the patient, he was already prepared for surgery. Since the area to be operated on was his right cerebellum, located in the back and bottom part of the brain (the most posterior and ventral part of the brain), the patient was positioned on his left side with his head propped up, so that the back right part of his head was accessible to the surgical team. He was completely covered in a sterile sky blue fabric material except for the section they were operating on. The initial incision had already been made when we were allowed to see him, and the inch of muscle and skin that cover that part of the head were held back by special surgical clips, revealing the bare skull beneath. The surgical auditorium, filled with students who had woken up before dawn to arrive at 6:30 am were previously chatty in somewhat excited suspense. Students now watched eagerly, in complete silence, in the darkened room.
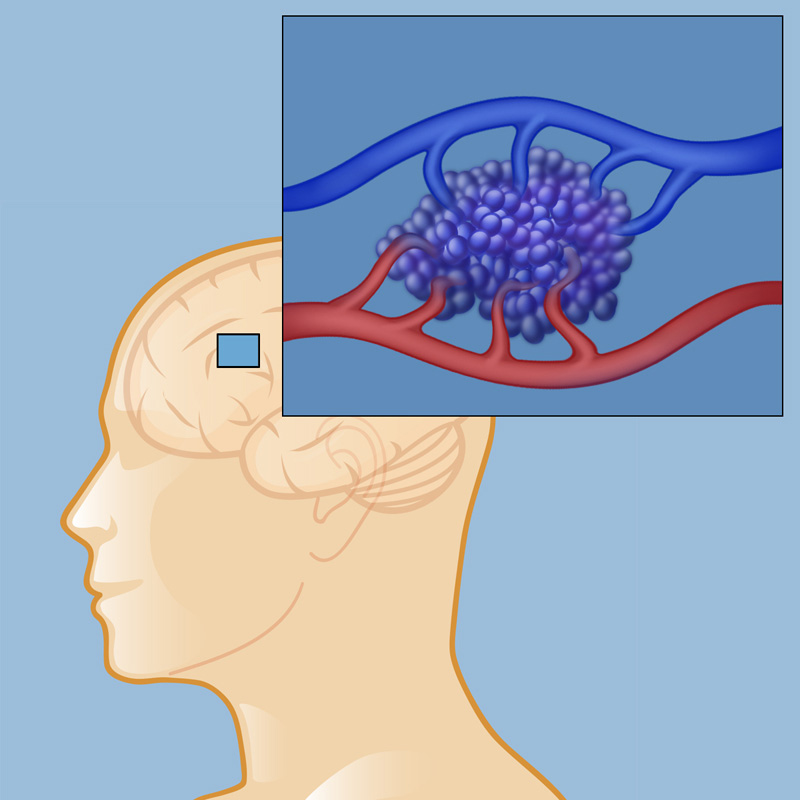
IMAGE SOURCE: Cavernous Malformations
A cavernous malformation is an abnormally formed blood vessel. Renowned for their fruit analogies, medical professionals compare cavernous malformations to mulberries, as their bulbous and bumpy appearance is reminiscent of a mulberry. Cavernous malformations are typically low pressure structures which swell with blood and can leak slowly, unlike an aneurysm which is more like a high pressure balloon which risks explosion. In either event, blood in the brain or spinal cord where it’s not supposed to be can cause serious damage to surrounding brain tissue. Leaked blood in the brain, called a hemorrhage, can possibly lead to a wide array of symptoms depending on where in the brain the hemorrhage is located – for example if there is hemorrhagic damage to Broca’s area and other regions in the left frontal lobe, a patient might experience difficulty or total loss of speech. Besides damage to brain tissue, bleeding in the brain can also lead to seizures due to iron deposits and the disruption of normal neural activity in that area; though interestingly, this is more of a concern with cortical bleeding, and not as likely to occur with bleeds in the cerebellum.
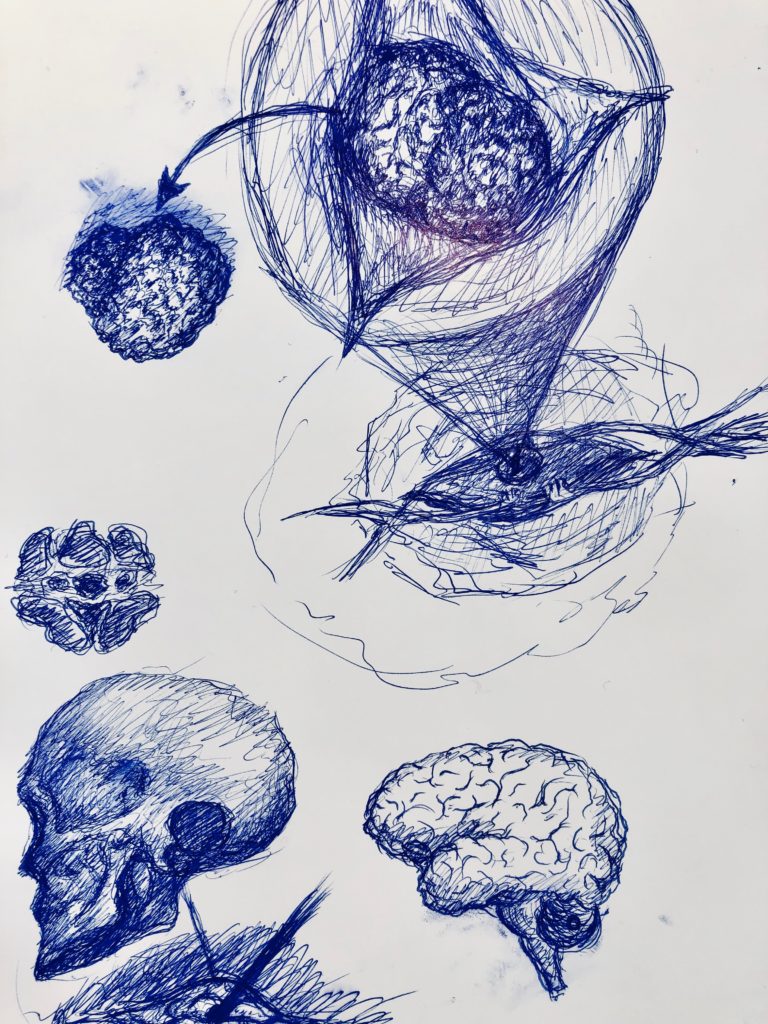
Sketch by NW Noggin Arts Coordinator Jeff Leake
LEARN MORE: Food eponyms in Pathology
LEARN MORE: Can Metaphors & Analogies Improve Communication with Seriously Ill Patients?
LEARN MORE: Iron in Chronic Brain Disorders: Imaging and Neurotherapeutic Implications
LEARN MORE: Brain iron redistribution in mesial temporal lobe epilepsy
LEARN MORE: Posttraumatic Epilepsy: What’s Contusion Got to Do With It?
The first stage of the operation we saw was the removal of an area of skull, which would be set aside and later replaced. A surgical drill was used to delicately carve out an area about the size of the cavernous malformation so that it could be pulled out of the void. As he was carving out the perimeter of the area of skull to be removed, a surgical assistant explained something that came as a surprise to many in the audience – that the surgeon can sometimes decide if they will replace the removed piece of skull or not.

IMAGE SOURCE: National Cancer Institute
A craniotomy is when a portion of skull is removed and then later replaced, whereas a craniectomy is when the skull cap is not replaced and the skin and muscle is sealed up directly over the meninges, the outer protective layers of the brain, without any skull piece returned beneath. In this surgery, Dr. Deshmukh opted for a craniotomy.

Many aspects of surgery, said Dr. Deshmukh, were “half art and half science.”
Once the skull cap was removed, the three outer protective layers of the brain were revealed – the dura mater, the arachnoid, and the pia mater, collectively known as the meninges. With the most delicate of movements and the most steady of hands, surgical scissors delicately clipped through these protective layers. As the meninges were slowly cut away, our first glimpses of actual brain tissue appeared.
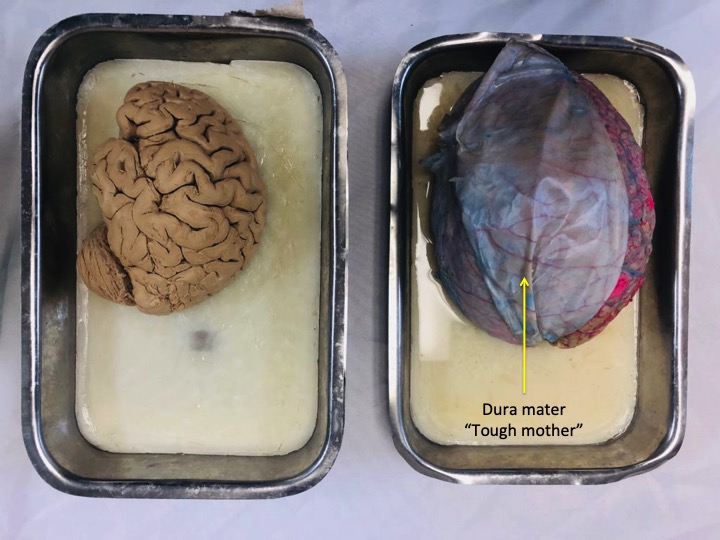
That tensile, vascularized flap over the brain is the dura mater (“tough mother”)
According to Dr. Deshmukh, the decision of whether or not to perform surgery to remove a cavernous malformation depends on several factors. One major factor in all brain surgery is the location of the malformation. This patient actually had hundreds of tiny cavernous malformations throughout his brain and spinal cord (two were removed from his spinal cord only a few months ago); however, the only one in the brain that had grown large enough to warrant a surgery was in his cerebellum. Fortunately for the patient, the cerebellum is a more forgiving region to operate on than most of the rest of the brain.
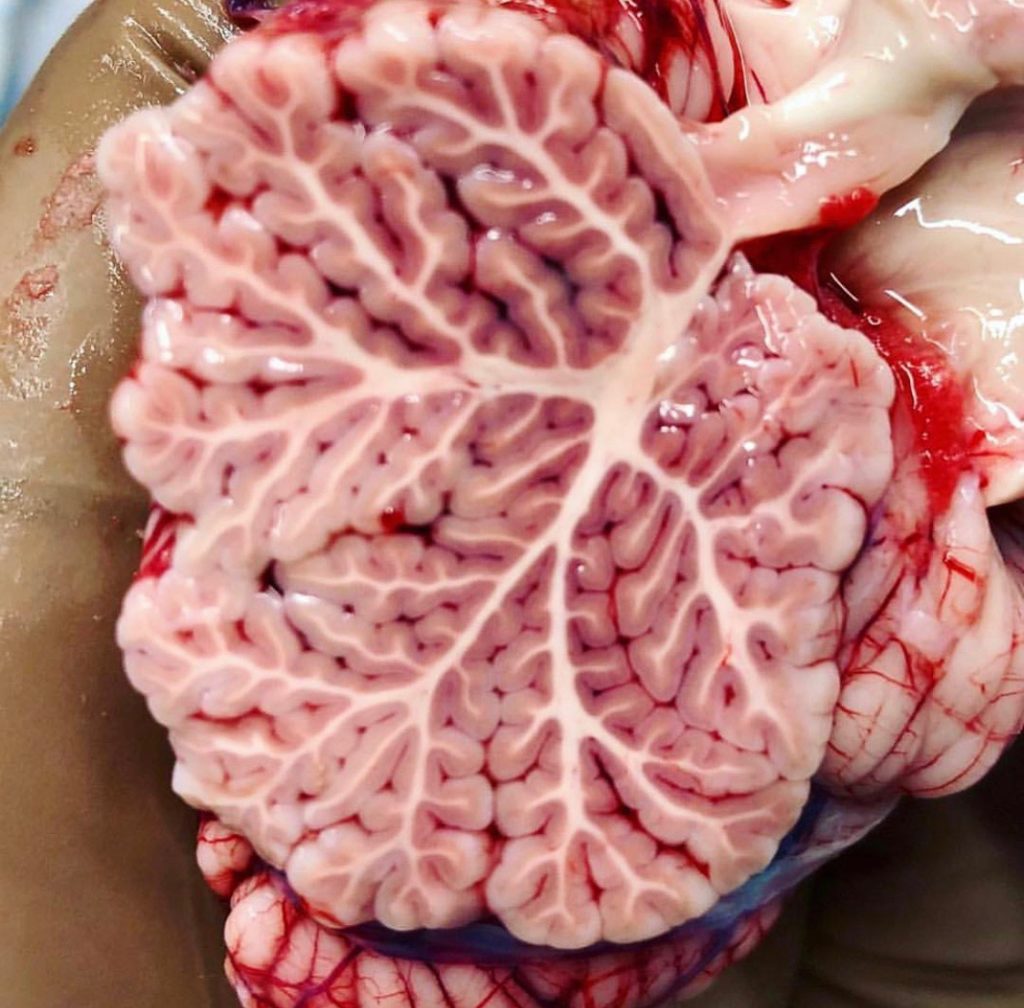
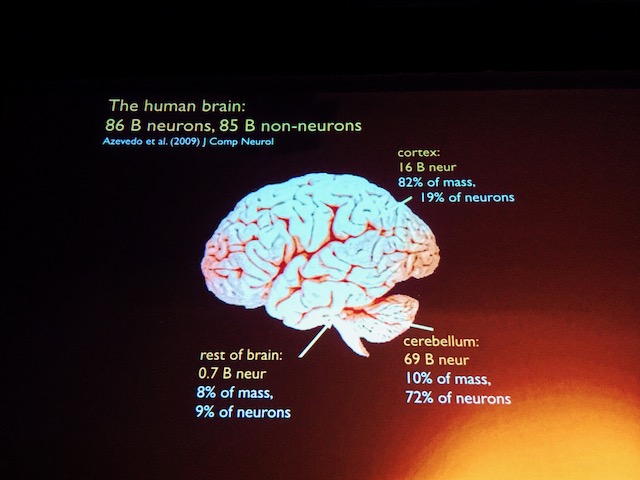
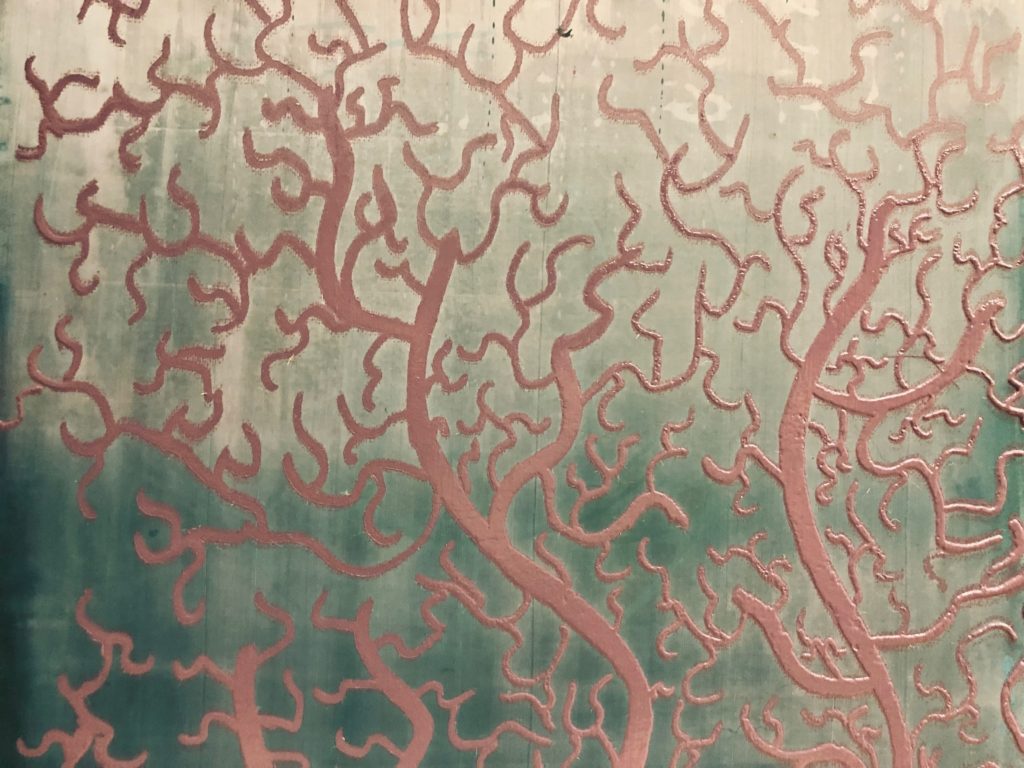
Beautiful image of the cerebellum by 123Anatomy_human321
Latin for ‘little brain’, the cerebellum contains the vast majority of brain cells (or neurons) in our nervous system – 60+ billion versus 16 billion in the human neocortex! Output for voluntary body movements originates in motor neocortex, in the fronntal lobe, but the cerebellum is important for coordinating movements with proprioception (awareness of where parts of the body are in space), vestibular information (balance, acceleration), and with more repetitive and corrective aspects of movement. Recent decades have shown that the cerebellum is also involved in learning and other functions.
LEARN MORE: Soup for Brains!
LEARN MORE: The role of the human cerebellum in performance monitoring
LEARN MORE: The Cerebellum’s Role in Movement and Cognition
In the operating room, the final portions of the meninges were finally cut. Under this layer, part of the cerebellum glowed pink under the surgical lights, and the cavernous malformation was clearly visible as a mulberry mess. It was clear to the audience which tissue was diseased – the malformation had an unhealthy, yellowish tint, and an unusual bumpy texture, compared with the smooth pink tissue of healthy brain. Some of the surrounding brain tissue was stained by the iron in the leaked blood from the malformation, causing permanent damage to some of the surrounding cerebellar tissue.

IMAGE SOURCE (note that this image is NOT from the Brain Watch patient): Surgical resection of intramedullary spinal cord cavernous malformations
At this stage of the surgery – the actual cutting away of the cavernous malformation, a surgical scope was used to zoom in closely to the area. The astonishing technology involved in brain surgery became apparent as staff rolled out a large futuristic looking machine. Accompanying the scope was a special chair the surgeon now sat in. Someone in the audience said the scene with all the special equipment and the surgical team dressed in their gear made it looked like something out of a sci-fi movie.

IMAGE SOURCE: (note that this image is NOT from the Brain Watch patient): Brain Surgery in 3-D: Coming Soon to the Operating Theater
Throughout the surgery Dr. Deshmukh used a special probe device that showed on a screen a 3D representation of the patient’s brain. Before the operation, 3D MRI scans had created an atlas of the patient’s brain, and when he placed the probe somewhere in the patient’s skull, it revealed on screen precisely where the probe was. Everyone in the audience could simultaneously see both the view from the scope and a monitor that showed where in the 3D brain atlas the probe was placed, as well as a view of the operating room.
In the operating room people wore special surgical clothes obscuring their faces and bodies, lending to the futuristic sci-fi atmosphere. I saw five people in that OR – a scrub technician in charge of the medical tools, a physician’s assistant who was next to the surgeon assisting his every move, an anesthesiologist, a circulating nurse who was there to leave the room and get things that were needed, and of course the neurosurgeon. In the audience, everyone’s eyes darted back and forth between the view from the surgical scope, the view from the interactive 3D brain atlas, and the view of the operating room.
Then came the most breathless part of the surgery – the cutting away of the cavernous malformation. Once more, surgical scissors were employed to delicately separate the tissue that connected the diseased portion from healthy brain. Since cavernous malformations are malformed vessels, it was intimately interspersed with healthy brain tissue, so great care was taken to minimize damage to the cerebellum.

First Dr. Deshmukh cut away the portion that was facing him, but eventually he had to cut the area behind the malformation which was obscured from view. To do this, he and the surgical assistant used tools to ‘roll’ the malformation towards him, so that he could see what he was cutting. As said, this is half art, half science, and his four years of university, four years of medical school, eight years of medical residency, and thirteen years of post-resident experience had trained Dr. Deshmukh to be skilled at just this sort of moment.
This delicate and careful cutting away of the malformation from the cerebellum under the scope was the lengthiest part of the surgery. The more cuts he made, the more free the malformation became. The entire time, the audience was completely captivated with eyes wide open.
Then, after hours of suspense, the climactic moment finally arrived! The surgical preparation, initial cuts, removal of skull cap, cutting of meninges, and cutting of brain tissue had built up to this monumental point – the actual removal of the cavernous malformation! The satisfaction of this moment is indescribable. After hours of preparation, the actual removal took about 10 seconds, but it was the. most. satisfying. 10. seconds. imaginable. One could vicariously feel the relief of 50+ years of a 2.4 cm abnormality in the cerebellum suddenly being pulled out after all that time. After all the cutting, it was as simple as taking forceps and simply pulling the loose darnn thing out!
After the most mesmerizing 10 seconds that have ever existed, the entire audience erupted with cheers and applause! Imagine the cheers and applause that happens at sports events, but instead of the stakes of the game being the winning of points, or touchdowns, the stakes in this game is the life and permanent brain health of a real human, physically and mentally. The very deepest core of what it is to be human is at stake. It’s hard to imagine anything as intense or exciting or satisfying as this masterful and dramatic performance. Waves of relief and exhilaration reverberated through the audience. Wow.
The rest the surgery had a more relaxed tone. It was almost hard to believe what we had just seen, and after the period of hyperfocus and hyper suspense which was a result of the high stakes of the surgery and the fact that we had been looking through the same zoomed-in scope that the surgeon was looking through, it now felt as if we came back to our senses, like waking up from an intense and vivid dream. We found ourselves once again aware of being in a surgical theater, watching a brain surgery.

The area that was formerly occupied by a cavernous malformation was cleaned with saline solution and surgical sponges. Then the meninges were sutured closed. At this point, the skull cap that had been sitting on a surgical table was readied for reattachment to the skull. Dr. Deshmukh used titanium plates called dogbone plates due to their shape to attach the skull cap back on, with the aid of titanium screws which were tightened by hand, without a machine. Then, the muscle and skin were sutured back together.

These days, brain surgeons don’t shave the patient’s head because this actually spreads more bacteria around, so this patient is able to conceal his stitches under his hair. This led to one of the strangest parts of the surgery – the part where they removed the sky blue medical fabric that had covered the entire patient except for the small area being operated on. Until then, we couldn’t see much of the patient, but then suddenly we saw the back of his head, his neck, his right shoulder, part of his right arm, and his upper back. Ohhhh, there was a person under there the whole time! It’s not clear which feeling is stranger – the feeling of suddenly seeing parts of a person that are normally visible (ie, not the skull and brain) after only seeing the inside of their skull for a few hours, or the the fact that it actually felt strange seeing part of their everyday body, and to us the inside of the skull had become ‘normal’ to see for a period of time.
LEARN MORE: Reducing Surgical Site Infections: A Review
LEARN MORE: The effect of hair on infection after cranial surgery
One must not forget that a surgery such as this is a team effort involving many specialists. Before and after the surgery, students in attendance were given presentations by various staff who worked at the hospital and were in some way involved in the treatment of this patient. They talked about the details and inspiration behind their role in the hospital, including a nurse practitioner, a physical therapist, a radiologist, a surgical physician’s assistant, a clinical research assistant, and a telehealth provider.

The surgery was a success! And the students in attendance learned immensely about the brain, the operation, and all the fulfilling career possibilities in the hospital that can be pursued. This was one of hundreds of cavernous malformations that Dr. Deshmukh and his team have removed, and it’s likely the patient will have a strong and brief recovery.
Many thanks to the surgical team and hospital for this unforgettable and educational experience.

LEARN MORE: Noggin @ BRAIN WATCH!
LEARN MORE: The scalpel raised


