Post by David Jacobs, Behavioral Neuroscience, OHSU

Neuroscience gets more complicated every day and the media does not always paint a detailed or accurate portrayal of what is being discovered. Thinking critically is a pivotal part of the scientific process, but the public is not always offered ways to assess findings. I hope to use this post to carefully guide readers through one research article. I will focus on highlighting the main findings, which address a critical public health issue and an issue in how we design experiments in neuroscience. I hope to help people feel less concern about approaching ‘dense’ scientific publications. You can learn this too!
Effect Selectivity
How do we as neuroscientists assess drug addiction in the lab? How can we use “models” we develop to predict if a treatment might work? Here I’ll focus on a paper that includes common animal models of addiction to assess a novel medication for tobacco (i.e., nicotine) addiction. I will go over some of the basic findings and tie it all to one important concept: the selectivity of an effect. This article itself is freely available and can be found here…
Detail from artwork by Christos Koutsouras
Quitting cigarettes can be hard, with frequent relapses. In fact only about 6% of smokers successfully quit each year, according to the National Institute on Drug Abuse (NIDA). Nicotine is one of the most dependence-provoking chemicals, particularly for teenagers, and it also primes the brain for dependence on other drugs of abuse, including cocaine, opioids and alcohol.
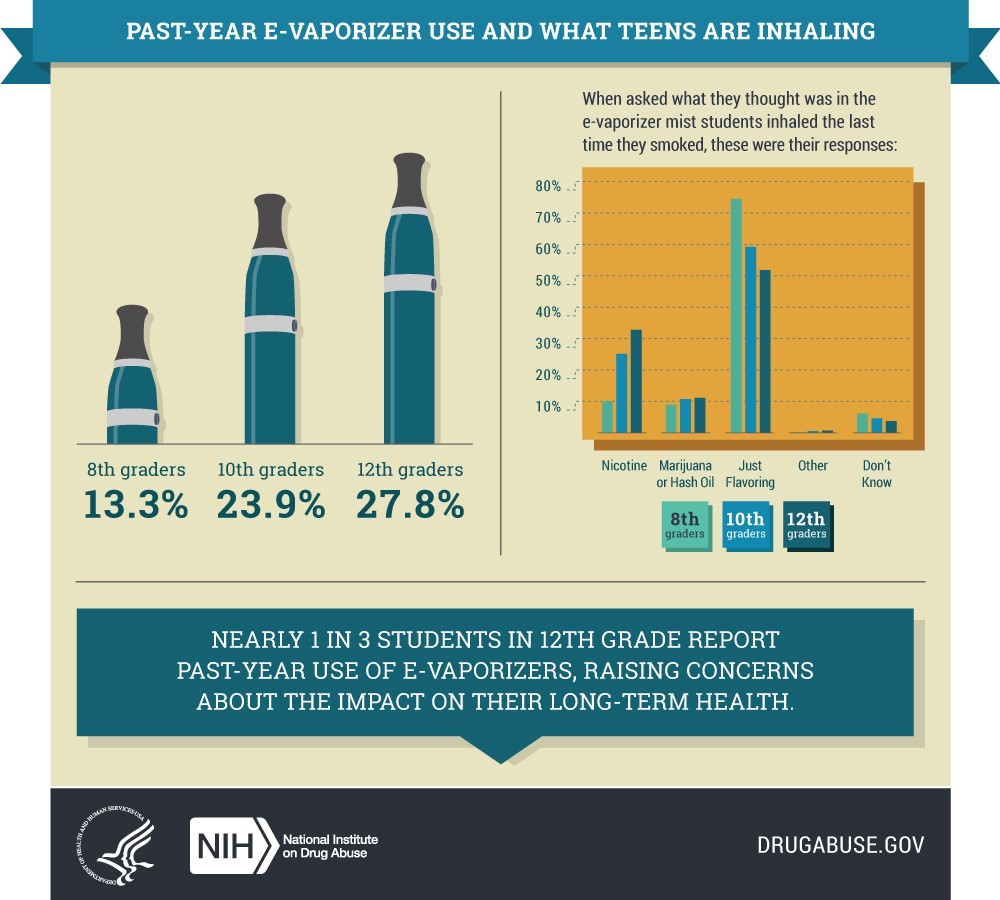
New methods of drug delivery are impacting adolescent exposure to nicotine…
LEARN MORE: NIDA: Is nicotine addictive?
LEARN MORE: Age of smoking initiation: implications for quitting
LEARN MORE: Vaping popular among teens; opioid misuse at historic lows
LEARN MORE: Comparative risk assessment of alcohol, tobacco, cannabis & other illicit drugs
LEARN MORE: A Molecular Basis for Nicotine as a Gateway Drug
So, the scientists in this paper are interested in looking at which treatments might help prevent relapse. Scientists have several ways of assessing both drug taking and drug relapse in animals, but the most prominent ones are drug self-administration and reinstatement.
It was discovered years ago that many mammals (and even pigeons!) will administer addictive drugs to themselves. That is, if you put a rat in a box (see below) with a lever, and every time the rat presses that lever they receive an injection of nicotine, the rat will learn that a lever response produces a drug injection. If the effects of the drug are reinforcing they will keep on pressing that lever. This procedure is known as drug self-administration and is considered the gold-standard of assessing a drug’s potential to be abused by the general population because drugs that animals will self-administer (including meth, cocaine, alcohol, and opioids) are also addictive in humans.
IMAGE SOURCE: Intravenous Self-Administration of Drugs of Abuse in Mice
Now that we understand self-administration, let’s look at another experimental approach used to model relapse, known as reinstatement. Reinstatement consists of two parts. The first part is extinction which is just like self-administration, only making a lever response does nothing (i.e., no drug injection). Initially the rat will still press the lever, presumably because it still expects a response will lead to nicotine and has not learned that the response no longer yields drug. However, the rat will eventually respond very little on the lever, as the rat has learned that the lever response no longer yields the drug injection. When this happens we say that the behavior has been extinguished.

Once the behavior is extinguished, the reinstatement phase of the experiment begins. Reinstatement is a return of drug seeking behavior in the presence of the drug or cues (like the lever) that predict the actual delivery of the drug. Reinstatement is argued to reflect some aspects of relapse because it assesses if exposures to the drug itself or cues associated with drug taking can bring back the extinguished response. This phenomenon is seen in the real world when exposure to just one cigarette or seeing an old friend who smoked cigarettes may drive a cigarette addict to smoke again (relapse). Thus if we can find ways to decrease or prevent the ability of a drug or drug-associated cues to reinstate responding for nicotine in rats, then the same treatment may prove useful in preventing this relapse behavior in humans.
To this point, Chantix (Varenicline), a FDA approved medication for quitting smoking, has been shown to both decrease nicotine self-administration and reinstatement in rats.
LEARN MORE: Treatment of nicotine dependence with Chantix (varenicline)
LEARN MORE: Varenicline for smoking cessation: efficacy, safety, and treatment recommendations

Cues associated with past consumption of alcohol can reinstate drinking behavior
LEARN MORE: Self-administration of drugs in animals and humans as a model and an investigative tool
Overview:
With that covered let us look at Figure 1, which provides the overview of the experiment:
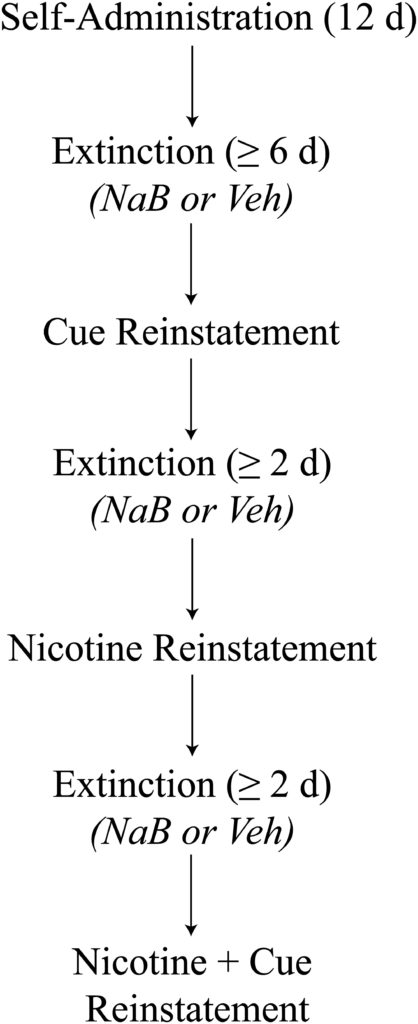
Rats are initially trained to press a lever to receive in injection of nicotine paired with a distinct cue light over 12 daily self-administration sessions. The authors then give a treatment drug that may be useful for preventing tobacco relapse called sodium butyrate, abbreviated as NaB.
NaB is in a drug class called histone deactylase inhibitors, abbreviated as HDACi. Discussing HDACi drugs is an article in itself, but briefly stated these are drugs that work through a process known as epigenetics, briefly discussed below.
LEARN MORE: What Do You Mean, “Epigenetic”?
LEARN MORE: Epigenetics across the human lifespan
In the image below you can see that DNA (the black line), which contains genes, is wrapped around protein complexes (the circles) called histones. When the DNA is wrapped tightly to these histones (e.g., on the right of the image) it cannot be accessed, so the genes will not be expressed.
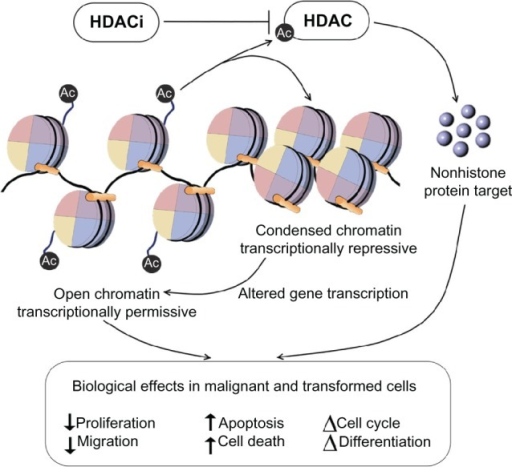
However, epigenetic factors like acetyl groups (denoted by “Ac”) can be attached to the histone, which loosens up the DNA, allowing the gene to be transcribed and whatever its protein product is to be built. What HDAC inhibitors (HDACi’s) like NaB do is inhibit HDAC’s, the enzymes that “de-acetylate” histones, which prevents the removal of these epigenetic factors, making the genes more accessible.
LEARN MORE: Roles of histone deacetylases in epigenetic regulation: emerging paradigms from studies with inhibitors
LEARN MORE: Histone deacetylase inhibitors (HDACIs): multitargeted anticancer agents
But why use a drug that increases DNA availability and gene expression for the treatment of tobacco addiction? HDACi’s increase protein synthesis, which is vital for learning and memory. Because relapse can be triggered by persistent memories of drug related cues and situations, the hope is that we can use these treatment drugs to re-learn associative drug cues and behaviors to prevent relapse. This is why the HDACi is used during the extinction phase of the experiment, because the HDACi should enhance what is learned during extinction and thus later decrease the reinstatement of drug-related responding.
Thus in the paper, the subjects experience the extinction phase either with or without the HDACi for several days until responding on the lever decreases to a standard predetermined level. After this, reinstatement is used to assess if the HDACi enhanced the alteration of these drug-associations.
Data:
There are quite a few symbols on the graphs. The symbols are designed to reflect the treatment the group received and whether the lever was active (led to drug) or inactive (led to nothing). Let’s just focus on the active lever responses (the filled in symbols). Remember, NaB is the treatment group (shown by circles) that received the HDACi treatment. Saline is a control group (shown by triangles) that did not receive HDACi but an equal exposure to what the drug was dissolved in (akin to giving someone a placebo pill). The NaB-6 h group got the HDACi treatment six hours after the extinction session and are shown by squares. This group is an important way to assess how selective this effect is to learning and memory. As I stated HDACi’s are thought to be useful for treating substance addiction because they may enhance learning and memory. Seeing as most of this learning and memory is going to take place 30-minutes after the extinction exposure takes place (a process known as memory consolidation) we would expect that the HDACi would only be useful if it were active when new memories were being processed and integrated into the brain. Thus, the NaB-6h group should look like the saline control group when tested in reinstatement.
So did the HDACi treatment do anything? Let’s look at figures 2A-D.
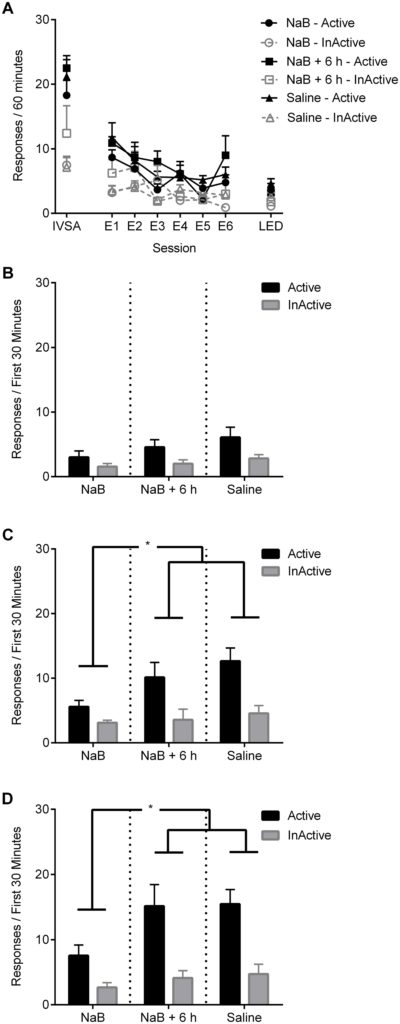
FIGURE 2: Assessment of NaB treatment during the extinction phase of the experiment on the reinstatement of responding for nicotine
Figure 2a shows us how many responses subjects made for nicotine injections on their last self-administration day shown by the data points above ‘IVSA’. Notice that the filled symbols are at about 20 responses (20 nicotine injections) per 60-minutes in the day before extinction and that all groups were responding about the same number of times for nicotine injections at the start. When we look at E1 (which stands for extinction day 1) we see that the number of responses drops to about 10 and continues to decrease to about 5 responses by the last extinction day labeled ‘LED’ on the graph. Also note that groups are all about equal over the extinction days. This shows that treatment with the HDACi did not do anything to the rate at which the drug-associated response was extinguished with these experimental procedures.
So what about reinstatement? Remember, this is our model of relapse. Reinstatement results are shown in figure 2B, 2C, and 2D below and the groups are now shown on the x-axis rather than by symbols. Also, active responses are shown by the black bars. Looking at figure 2B, where the nicotine cue light was presented, we see the NaB group responded less than the other groups when the cue light was presented. However, this result is not statistically significantly different from the other groups (discussed below), suggesting that the HDACi did not impact a cue-induced relapse-like behavior. Figure 2C however shows responding when a single nicotine injection was given before the session began. The responding is now different between groups as indicated by the *. The * typically means a significant difference between two groups. This is determined by statistical tests scientists perform to see if the differences they see are likely due to their manipulation (in this case the HDACi treatment) or just random chance. According to Figure 2C the NaB treatment group responding was significantly less than the NaB-6 h and control saline group. This same effect is observed in figure 2D when a cue presentation and nicotine injection were given. These figures suggest that treatment with a HDACi only during important periods for learning and memory can decrease the reinstatement of responding, i.e. it decreases relapse-like behavior, for nicotine.
One more consideration:
We thus may speculate that this drug shows some potential to prevent relapse in some instances. However there is one big issue to consider; the issue of selectivity. Treatments can have effects that influence how something behaves without directly affecting the thing we care about (addiction-related behavior). Consequently, we want to know not only if a treatment appears to work, but if it works by impacting the drug-response behavior or by generally making it so animals don’t want to respond.
Brain cake by NW Noggin volunteer Kateryna Bondarenko
For example, say you eat Food A and it makes you feel sick. Then immediately after this someone offers you cake (assuming you like cake), and you say no. Now one could think ‘Wow, Food A prevents the liking of cake.’ However, your liking of cake is probably the same, you are just not in the mood. Food A did not have a selective effect on cake it just made it so you didn’t want to do anything. The same could be happening in this study. The HDACi may be making the animals feel uncomfortable and they may begin to associate the responding and context with that feeling. Consequently, when they are given something that should make them seek nicotine they do not because they feel uncomfortable in that context due to the treatment. This is the issue of selectivity and it is something to look for in any scientific finding. It is always important to ask if the effect something has on behavior is specific to that behavior or if it just generally alters behavior.
Appropriately, the authors address this in this paper. If we skip figure 3 and go to figure 4 we will see a set of graphs that looks very similar to what we saw in figure 2. However, this time instead of training rats to press a lever for nicotine they now press a lever for food, a natural reward. This experiment provides an assessment of if the HDACi treatment affects the general lever-pressing behavior that is required to get nicotine in this study.
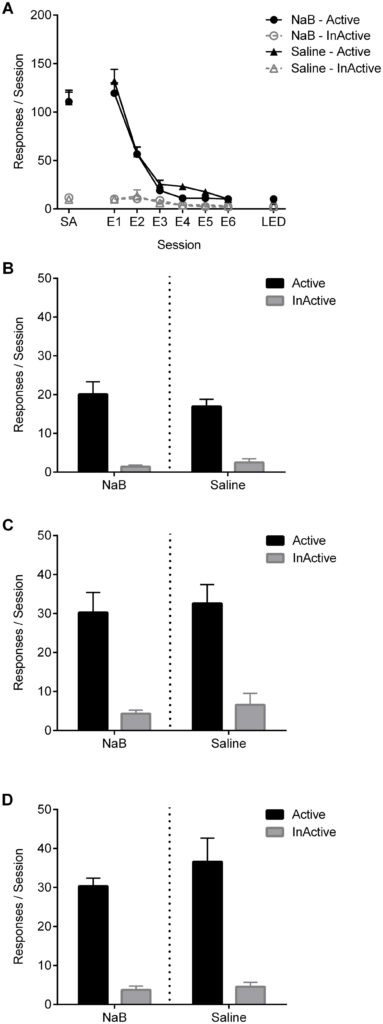
FIGURE 4: Assessment of NaB treatment during extinction on reinstatement of responding for food (is the effect of NaB treatment selective for nicotine?)
Focusing on the filled symbols in figure 4A (above) one can see that responding decreased during extinction (E1 through LED on the x-axis) for both the HDACi and saline groups, just like what we saw with nicotine in Figure 2A. However, when we look at Figures 4B, 4C, and 4D below we see that the HDACi group did not differ from the control group when reinstatement was performed with either the food cue, food, or both. This is different from the results obtained when responding was for nicotine and shows that the general response behavior was not impacted by the HDAC.
If the HDACi did affect general behavior required to respond we likely would have seen a difference between the HDACi and NaB groups during reinstatement for Figure 4. Since we did not see this we can conclude the ability of HDACi treatment to decrease the reinstatement of responding for nicotine was selective for nicotine administration in this study.
There are certainly many other things that could be discussed in this paper, but these results illustrate a nice point in evaluating selectivity at two levels. First the authors assess if the effect was actually happening in a time period relevant to learning and memory as hypothesized. Second, the authors assess if the effect was due to general decreases in motor behavior or nicotine specifically. Thus, it seems the HDACi does decrease the reinstatement of nicotine seeking under some conditions and only when given in critical periods for learning and memory.
Will this show consistent utility in preventing smoking relapse with humans? That is something that will take time to figure out, but this paper provides a brick for the house that we are trying to build.


