Post by Meaghan Creech, undergraduate in Public Health: Pre-Clinical Health Sciences pursuing a Neuroscience Minor at Portland State University. Meaghan is currently in the last term of their NIH-funded PSU URISE Cohort 2 placement in Nicole Bowles Lab within the Oregon Institute of Occupational Health Sciences at Oregon Health and Science University.
If you want to participate in the ongoing (currently summer 2024) study mentioned in this post, please check out the eligibility criteria and fill out the screening survey to see if you qualify.
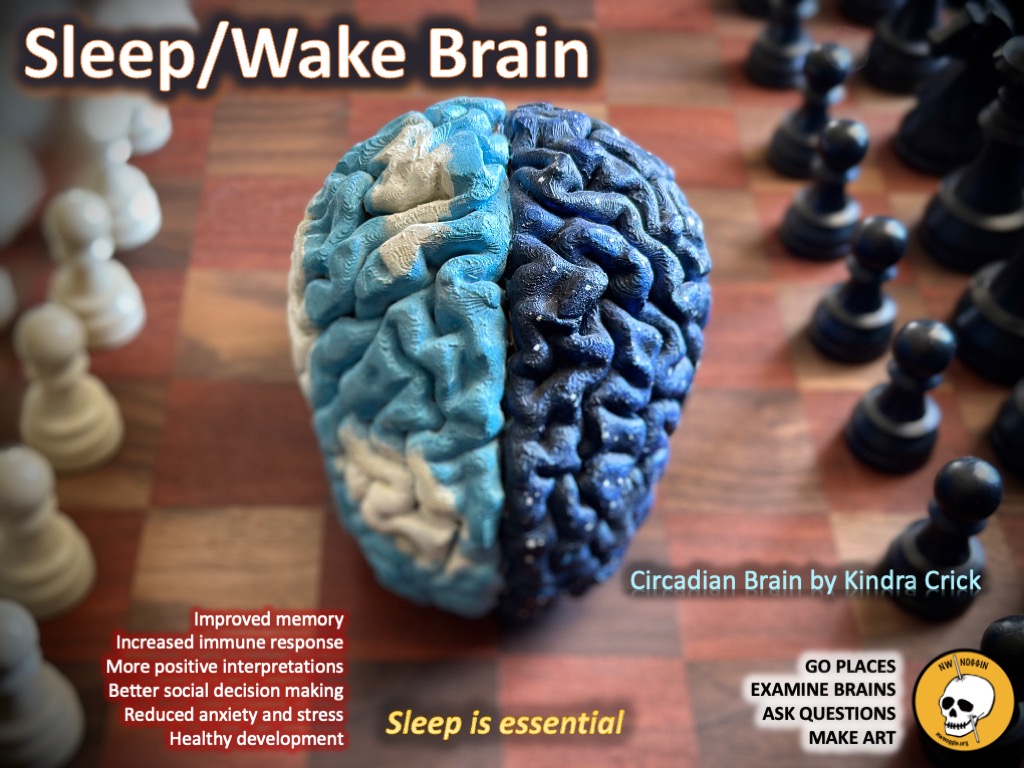
Sleep is important
Everyone sleeps.
We sleep (eventually) even when we try to stay awake, and even if we don’t entirely understand why. We do it even though it’s pretty time consuming, and we do it even when it doesn’t always do for us what it’s supposed to do (though what sleep is supposed to do for us is, weirdly enough, still up for debate).
LEARN MORE: Exploring phylogeny to find the function of sleep
LEARN MORE: Noggins in Nod: The Science of Sleep
LEARN MORE: Why Is Sleep Important?
What is sleep apnea?
Yet not everyone sleeps well. Sleep apnea falls under the umbrella of what is called sleep-disordered breathing, and despite having a technical name that you might not have heard before, you almost certainly know someone who has sleep apnea. This person might even be you!
Do you know anyone who snores?
Snoring is one of the indicators most commonly associated with sleep apnea.
Snoring is both a loud and obvious clue (for people who sleep within earshot) and a challenge to one’s social life, especially to maintaining relationships with people who might sleep nearby, for whom your snoring might be noise pollution contributing to their own disturbances in sleep.
However, snoring is very prevalent, and doesn’t always point to sleep apnea. You can be someone who snores and doesn’t have sleep apnea, and you can be someone who has sleep apnea and doesn’t snore.
LEARN MORE: Snoring: a source of noise pollution and sleep apnea predictor
History of sleep apnea
Judging by the many references in art, literature, and recorded history to the signs, symptoms, and experiences associated with sleep apnea, it’s clearly not a new condition.

IMAGE SOURCE: The Nightmare by Henry Fuseli
Henry Fuseli’s painting “The Nightmare” shows us an image of a sleeping person with a non-human being perched on their torso, facing the viewer. This painting is often associated with sleep paralysis, another sleep disorder that can be caused by sleep apnea (but can also occur in isolation or with other sleep disorders). Sleep paralysis as a consequence of sleep apnea has been, understandably, linked to both bedroom avoidance behavior and bedtime anxiety.
LEARN MORE: Recurrent fearful isolated sleep paralysis – A distressing co-morbid condition of obstructive sleep apnea
LEARN MORE: Sleep Paralysis, a Medical Condition with a Diverse Cultural Interpretation
LEARN MORE: Sleep Paralysis
Do you feel “hagridden?”
The term hagridden breaks down into the words “hag” and “ridden.”
From words like “bedridden” we can extrapolate its meaning, but it’s worth considering why this word has been used to describe sleep issues going back to at least 1677. The word hag points to witches, and ridden (in combination with hag) points not to the creepy piggyback rides I envisioned as a child when I first heard the term, but to the pervasiveness of the issue and the severity of its impact on someone’s life.

SOURCE: Google on “hagridden”
For centuries, some people have reported feeling “oppressed, dominated, or plagued by” the hags (demons, harpies, or witches) to whom they attributed their issues with sleep.
LEARN MORE: The Old Hag phenomenon as sleep paralysis: a biocultural interpretation
LEARN MORE: Witchcraft beliefs around the world: An exploratory analysis
Do you have sleep apnea?
So let’s say that you’re sleeping over at your friend’s house.
You’ve eaten all the snacks, played all the games and now the movie credits are rolling, and your friend is already asleep. You’re really tired, too. You get ready for sleep (track down the remote and turn off the TV, plug in your phone, pull up the hood and pull down the sleeves to your hoodie because your friend forgot to give you a blanket) – when you notice that it’s weirdly quiet.
STOP BREATHING

You look at your friend, who’s kind of a loud sleeper (he gets in trouble at school more than anyone else in your friend group because even though you’ve all fallen asleep in class, he’s the one your teacher can hear sleeping). He looks fine, and he seems asleep (though you worried he might have woken up while you were rustling around for the remote and your phone charger).
However you notice that he does not seem to be breathing; his chest isn’t moving, and you’re not hearing him breathe even though he has a small room and you’re pretty close to each other in front of the TV, so that y’all could keep the volume low enough and not wake up his family.
Is the sleep of someone you know ever suddenly so silent that you wonder if they’re still breathing?
GASP

You’re starting to get worried, and you think about getting up to help, which is right when your friend takes a deep, loud, dramatic gasp of air. Like, it’s so dramatic that you laugh because you think he was actually awake and it was a joke, like the noise zombies sitting up out of coffins make in B horror movies.
Your laugh wakes your friend up, and he’s confused and kind of irritated, and asks what you’re laughing about. You tell him, and he just looks at you like you’re weird (which you’re starting to feel you are), and tells you to go to sleep and then rolls onto his side and goes back to sleep himself.
Do you ever wake up short of breath and rapidly inhaling? Are you “air-hungry?”
SNORT
You’re both asleep for a while, and then something loud wakes you up.
You’re not sure, because you’re really tired (your phone says it’s 3:00AM), but you think you heard a snort, like when somebody laughs so hard they snort, only you didn’t hear any laughing. Your friend is awake, too, and you ask him if he heard something. He looks irritated but also a little scared, and says that he thinks so but he’s not sure. You both listen for a while and then go back to sleep.
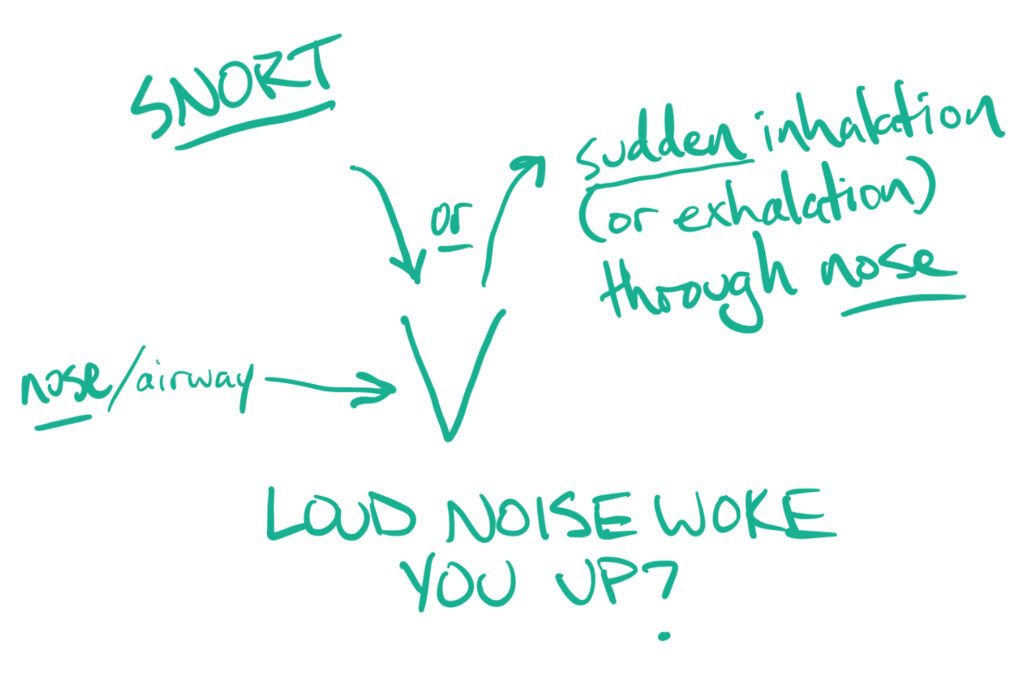
When you get up in the morning, your friend seems really tired, which is weird because he went to sleep before you did.
GROAN
You might have heard people groan in their sleep. This groaning is called “catathrenia.” Catathrenia has only recently been considered in the context of academic sleep medicine, with the first PubMed mention in 2001, though historical mentions appear as early as 1688.
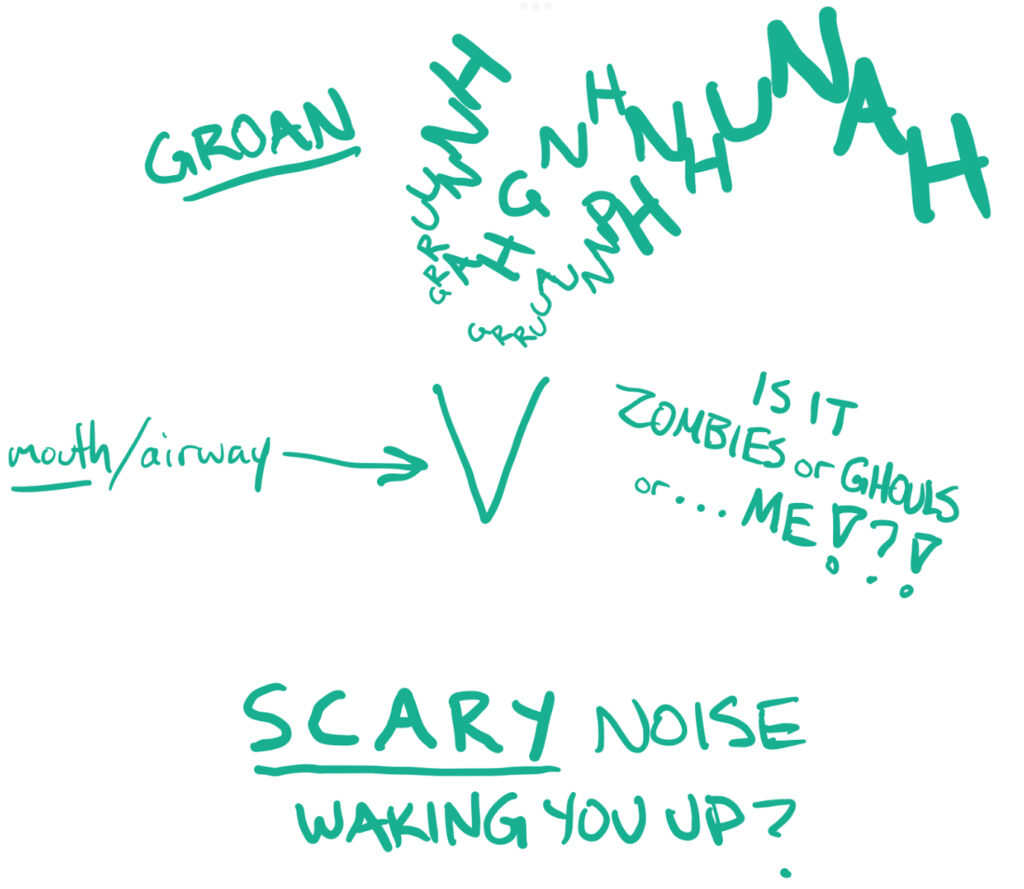
Your respiratory drive ensures that you keep breathing (whether you’re thinking about it or not). It depends on information about the balance of oxygen and carbon dioxide in your blood. Your brain and your lungs work together to keep your body in homeostasis so that you can keep on keeping on.
The groaning is thought to be caused by disruption of the internal respiratory drive, and can be another noisy symptom of sleep apnea. Some researchers, however, think it is a separate parasomnia of its own.
LEARN MORE: Parasomnias
LEARN MORE: ‘Nocturnal groaning’: just a sound or parasomnia?
LEARN MORE: The curious incident of groaning in the night-time
LEARN MORE: Catathrenia in severe obstructive sleep apnea: A novel entity never described before
LEARN MORE: Catathrenia (nocturnal groaning): A new type of parasomnia
LEARN MORE: Continuous positive airway pressure as treatment for catathrenia (nocturnal groaning)
LEARN MORE: Catathrenia (nocturnal groaning): an abnormal respiratory pattern during sleep
LEARN MORE: Breath holding – A rapid eye movement (REM) sleep parasomnia (catathrenia or expiratory groaning)
LEARN MORE: Catathrenia: A rare parasomnia which may mimic central sleep apnea on polysomnogram
LEARN MORE: Catathrenia: Parasomnia or Uncommon Feature of Sleep Disordered Breathing?
Do you wake up abruptly or does someone hear you snort yourself awake?
HEAR A LOVED ONE STOP BREATHING?
Until they can seek treatment, wake them up!
This minimizes the amount of time they go without air, and going without air causes health issues.
Do you wake up tired every day and feel like your sleep isn’t restful? Get a sleep study!

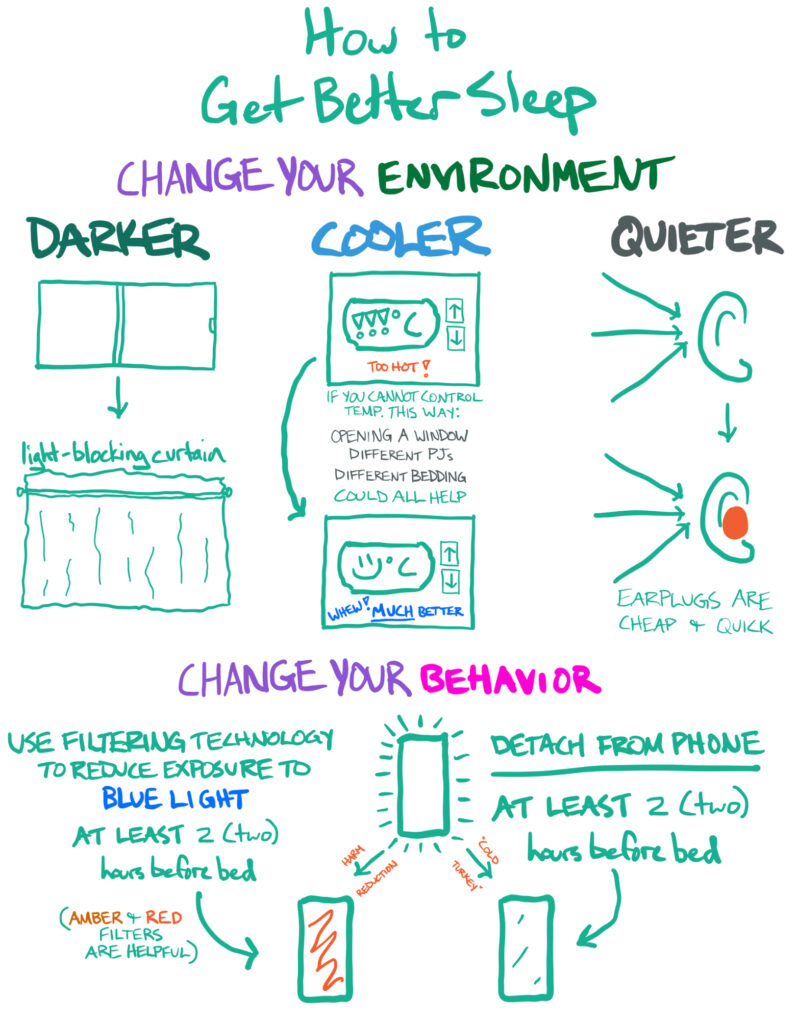
Clean up your efforts to sleep
You should also improve your sleep hygiene (the technical term for how you accommodate your sleep and prepare for sleep behaviorally). Avoid known causes of sleep disturbances or extra inflammation, elevate your head, and make your sleep space as cool, quiet, dark and comfortable as possible.
LEARN MORE: The Good, The Bad and the Ugly of Inflammation
LEARN MORE: Why all the buzz about inflammation — and just how bad is it?
THOUGH BE AWARE: Even if you or someone you know exhibits ALL of these symptoms – stopped breathing, gasping, snorting and groaning – you could still have something other than sleep apnea. It’s important to seek assessment and, if necessary, care from a qualified professional.
Need a sleep study? These organizations can help!
Providence Sleep Disorders Center
The Portland Clinic Sleep Center
The Oregon Clinic Sleep Medicine
Here are the online search terms I would recommend if you are looking for help outside the Portland, Oregon region and are concerned that you or someone you know might have sleep apnea or another sleep disorder: “sleep study” + [name of city/town where you’d be seeking care]; “sleep specialist” + [name of city/town where you’d be seeking care]
You can also ask your primary care provider for more information and/or a referral; sleep studies are more accessible than they used to be, and many people will have the option to access equipment that they can wear at night in the comfort of their own homes to assess their breathing while asleep.
Our study is recruiting right now at OHSU!
If you are between the ages of 21 and 35 and you want to participate, you can see if you’re eligible by taking this pre-screen survey. If you don’t qualify for this study, there are others; check this website for other studies at OHSU that you might be eligible for now or in the future.
Types of sleep apnea
There are multiple types of sleep apnea.
The most common is obstructive sleep apnea (OSA). Central sleep apnea is less prevalent than obstructive sleep apnea, but because treatments can vary, an accurate diagnosis is important.
Obstructive Sleep Apnea is characterized by airway collapse and is often associated with higher body mass index (BMI). However, it is also very common in people with connective tissue disorders that impact collagen matrix formation due to lack of adequate structural support for the airway.

LEARN MORE: What Is Sleep Apnea?
LEARN MORE: A comprehensive review of obstructive sleep apnea
LEARN MORE: Diagnosis and management of obstructive sleep apnoea in adults
LEARN MORE: Obstructive Sleep Apnea: Women’s Perspective
LEARN MORE: Analysis of behavioral problems in children with sleep-disordered breathing and decreased REM sleep
LEARN MORE: The Extracellular Matrix of the Lateral Pharyngeal Wall in Obstructive Sleep Apnea
LEARN MORE: Central sleep apnea: misunderstood and mistreated!
Health Consequences of Untreated Sleep Apnea
The way you breathe while sleeping has body-wide, long-term impacts.

IMAGE SOURCE: Richard T. Jones Hall for Basic Medical Sciences
Hypoxia due to apnea: Insufficient O2 or excess CO2
Many of the health consequences of untreated sleep apnea are downstream consequences of the lack of sufficient blood oxygenation that occurs when someone can’t breathe while sleeping.
Some of the known risks involved with chronically untreated sleep apnea include an increased tendency to develop cardiovascular disease and an increased tendency to develop neurocognitive issues due to a lack of sufficiently oxygenated blood to supply the heart, circulatory system, brain and other organs.
LEARN MORE: Brain Circuitry for Arousal from Apnea
LEARN MORE: Hypoxic Burden in Obstructive Sleep Apnea: Present and Future
LEARN MORE: Hypoxia and Sleep-disordered Breathing: Friend or Foe?
LEARN MORE: The efficacy of antihypertensive drugs in chronic intermittent hypoxia conditions
Cardiovascular disease risks due to untreated sleep apnea
Your heart and your vascular system (the system that transports your blood throughout your body so that it can supply sufficient oxygen to your tissues) depend on there being enough oxygen in your blood to meet the body’s needs.
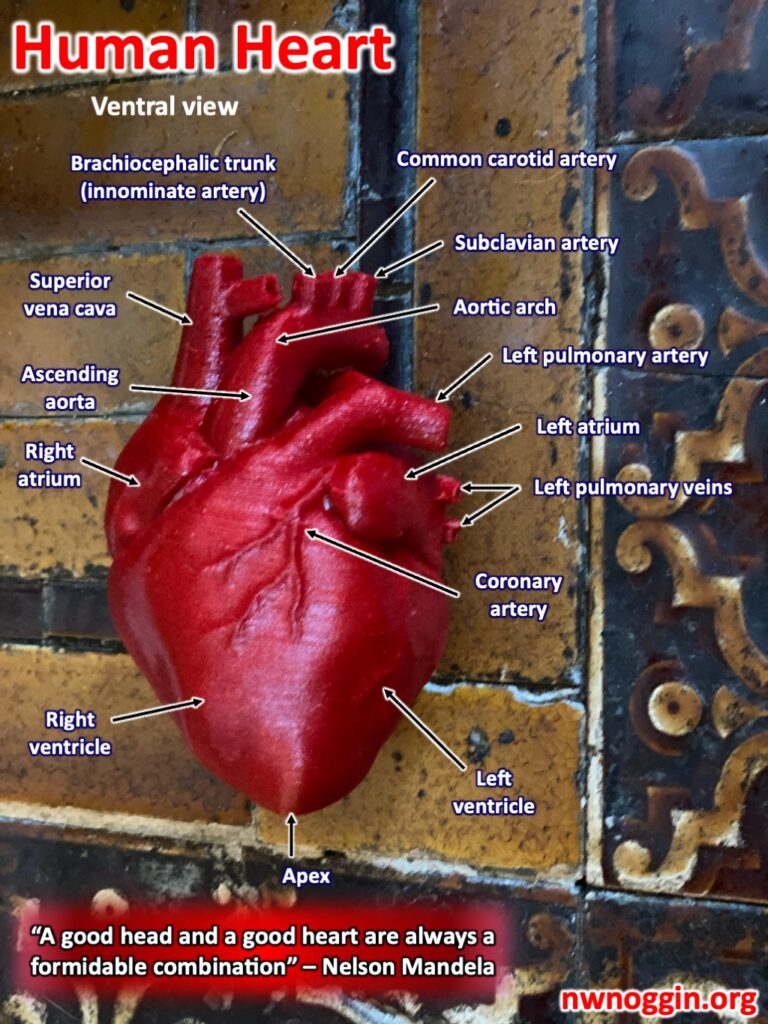
When this is not the case, cardiovascular disease can result. It’s important to get checked out if you have concerns about your heart health (whether or not you have sleep apnea), but it’s especially important to care for your heart if you do have sleep apnea because of the increased risk of cardiovascular disease.
LEARN MORE: Sleep Apnea and Sudden Cardiac Death
LEARN MORE: Inflammation in sleep apnea: an update
LEARN MORE: Obstructive Sleep Apnea Phenotypes and Markers of Vascular Disease: A Review
LEARN MORE: Cardiovascular Disease in Obstructive Sleep Apnea: Putative Contributions of Mineralocorticoid Receptors
LEARN MORE: Sleep-disordered breathing and cardiovascular disease
LEARN MORE: Obstructive sleep apnea and stroke
Neurocognitive consequences of apnea
Your brain and nervous system also need sufficiently oxygenated blood to function well.
My own CPAP machine has needed replacement supplies for a while, and finally receiving them made it miles easier to do the thinking involved in both my homework and my research. If you sometimes feel like things are more difficult cognitively after a bad night’s sleep, just imagine a lifetime of nights with only bad sleep and you’ll understand why treating sleep apnea is so important.
LEARN MORE: The relationship between inflammation and neurocognitive dysfunction in obstructive sleep apnea syndrome
LEARN MORE: Sleep, Health, and Society
LEARN MORE: Obstructive Sleep Apnea is Linked to Depression and Cognitive Impairment: Evidence and Potential Mechanisms
LEARN MORE: Obstructive sleep apnea and neurocognitive performance: the role of cortisol
LEARN MORE: Role of Oxidative Stress in the Neurocognitive Dysfunction of Obstructive Sleep Apnea Syndrome
LEARN MORE: Obstructive sleep apnea and neurocognitive function in a Hispanic/Latino population
LEARN MORE: The association between sedentary behavior and obstructive sleep apnea
How do you treat sleep apnea?
CPAP (Continuous Positive Airway Pressure) machine
“CPAP (continuous positive airway pressure) is a machine that uses mild air pressure to keep breathing airways open while you sleep.”
— CPAP, from the National Institutes of Health

One concern about CPAP devices is the purportedly low compliance rate.
People don’t always wear their masks, and it can’t help if it’s not being worn. Luckily, those of us who need it the most are more likely to be sufficiently compliant to get significant benefit from wearing the mask. I was resistant at first, but once I experienced the relief of restorative sleep I was sold, and I’ll never go back.
Worries about dating and/or bed-sharing can be one of the obstacles to compliance, but fear not! Modern CPAP devices are surprisingly quiet and come in a wide variety of designs and sizes, so you can Goldilocks your way to a great fit. Getting good sleep in a sleek new piece of headgear will feel miles better than getting bad sleep without it.

Mask designs vary, and they come in different sizes.
I use the smallest size in my mask design, which covers both my nose and mouth, but many designs only cover the nose (if that’s more physically or psychologically comfortable for you). Only use distilled water in your CPAP’s water reservoir, as there are health risks associated with using water that is not distilled.
BIPAP: Alternative to CPAP
In some cases, CPAP might not be effective.
BiPAP (BiLevel Positive Airway Pressure) is an alternative treatment that looks similar to CPAP but works slightly differently. Where CPAP uses only one positive pressure (“pushing” air into the airway based on the needs of the person wearing the device), BiPAP uses two positive pressures, one of which is higher than the other. The higher pressure is similar to the positive pressure used in a CPAP device and is used on the inhale, while the lower pressure is used on the exhale. This additional respiratory support can help satisfy respiratory needs during sleep in cases where CPAP alone would not.

IMAGE SOURCE: How To Know if You Need a BiPAP Machine
LEARN MORE: CPAP and Bi-level PAP Therapy: New and Established Roles
LEARN MORE: Is bilevel PAP more effective than CPAP in treating hypercapnic obese patients with COPD and severe OSA?
Cannabis
What impact does cannabis have on sleep?

Front, L to R: Aanu Ayeni, Nicole Bowles, Joshua Gonzalez, Meaghan Creech
Back, L to R: Omar Ordaz Johnson, Ayeisha Haswarey, Latroy Robinson (Aug 2022)
For the past two years, I’ve conducted research on cannabis and sleep, and to be clear about the nature of the work, it has nothing to do with sleep apnea aside from the references to sleep apnea treatments I’ve encountered at conferences and in papers presented in our OHSU journal club.
Our research is ongoing, and recent discussion about the federal rescheduling of cannabis might accelerate advancements in the field, but the disappointing reality of past and current restrictions on researching the human health impacts of the naturalistic use of cannabis in the United States is that there is a dearth of studies that attempt to answer questions about the potential benefits of cannabis for treating sleep disordered breathing.
LEARN MORE: Schedules of Controlled Substances: Rescheduling of Marijuana (DEA)
The effects of cannabis on sleep remain uncertain.
As of 2018, the AASM (American Academy of Sleep Medicine) offered a position statement that dronabinol (the synthetic THC that is one of the ways to study THC/cannabis in U.S. laboratories) is not approved by the FDA for treatment of obstructive sleep apnea, and that “medical cannabis and/or its synthetic extracts should not be used for the treatment of OSA due to unreliable delivery methods and insufficient evidence of effectiveness, tolerability, and safety.”
LEARN MORE: Medical Cannabis and AASM Position Statement: The Don’t Ask, Don’t Tell Wishing Well
Yet there is more and more interest in expanding treatment options as awareness of sleep apnea grows. Whether or not the AASM ever changes their ruling, people in need of relief from symptoms that are downstream consequences of sleep apnea will seek that relief in a variety of forms, and cannabis is increasingly accessible relative to other commonly prescribed palliative medications like opioids and anxiolytics. If I had to guess, I’d say the average sufferer would pick relief over AASM compliance; this seems like a place where science rubber meets science road.
LEARN MORE: Effects of Cannabinoids on Sleep and their Therapeutic Potential for Sleep Disorders
LEARN MORE: Clinical Management of Sleep and Sleep Disorders With Cannabis and Cannabinoids
LEARN MORE: Cannabinoid Use and Obstructive Sleep Apnea: A Retrospective Cohort Study
LEARN MORE: Medicinal cannabis improves sleep in adults with insomnia
LEARN MORE: The Effects of Cannabinoids on Sleep
There is evidence to suggest that the stigma and complex legality associated with the use of cannabis as a medicine sometimes impacts access to effective healthcare due to cannabis’s current status as a Schedule I controlled substance.
LEARN MORE: Perceived Stigma of Patients Undergoing Treatment with Cannabis-Based Medicinal Products
LEARN MORE: The role of stigma in cannabis use disclosure: an exploratory study
LEARN MORE: A qualitative review of cannabis stigmas at the twilight of prohibition
Some of the effects of cannabis consumption that might appeal to recreational cannabis consumers are also seen as drawbacks by medical cannabis consumers. These effects include but are not limited to the associated cognitive detriments, one of the more common of which is short-term memory loss.
LEARN MORE: The short-term and long-term effects of cannabis on cognition: recent advances in the field
LEARN MORE: Relationship Between Cannabis Use and Immediate, Delayed, and Working Memory Performance Among Older Adults
Another important consideration are the long-term health detriments that can be a downstream consequence of cannabis consumption, depending on modality of consumption; combustion remains the riskiest way to consume cannabis due to the carcinogenic effects of the tars produced when burning and inhaling any plant matter.
LEARN MORE: Cannabis and Lung Health: Does the Bad Outweigh the Good?
LEARN MORE: Smoking cannabis associated with increased risk of heart attack, stroke
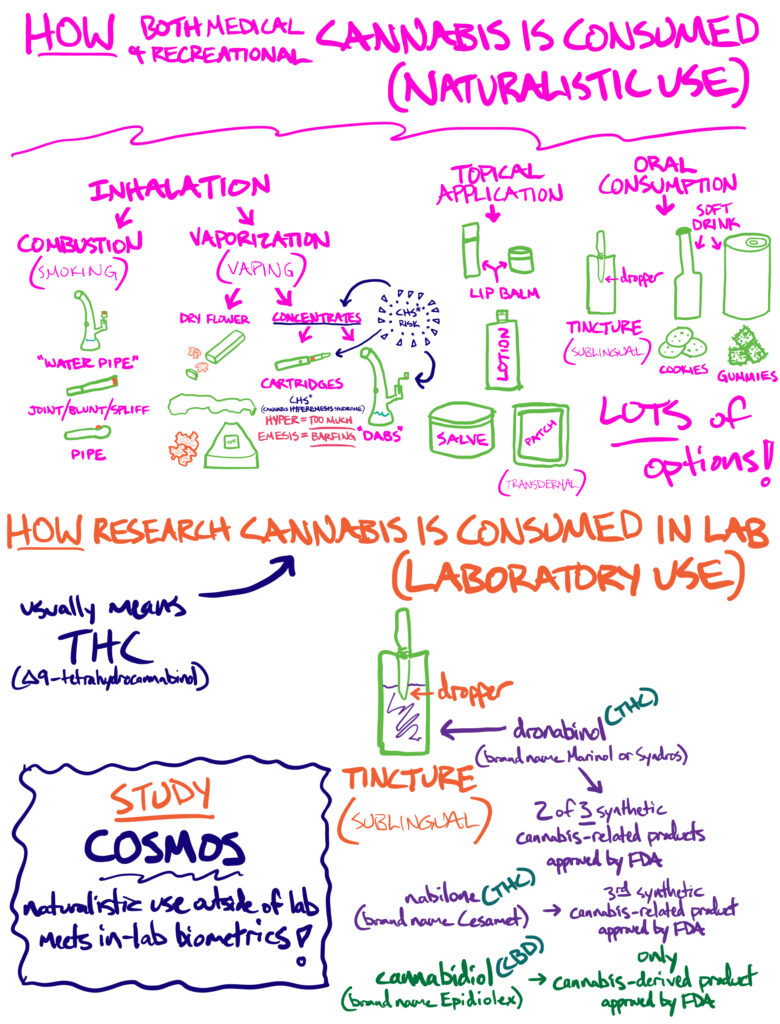
In addition, most research into cannabis has been funded by NIDA (the National Institute on Drug Abuse) so the knowledge base we have about its effects is limited in scope by NIDA’s mission, and by research use of limited drugs like dronabinol, which contain only one cannabinoid (THC), as opposed to the more complex mix of cannabinoids and other chemicals found in the plant that people actually use.
The effects of cannabis on human sleep are still uncertain due in part to these constraints, but there is hope that with the DEA’s proposed rescheduling of cannabis from Schedule I to Schedule III, new opportunities to learn more about how cannabis affects the human brain and body will appear.
LEARN MORE: Cannabis Science Interest (CSI) Group @ NIDA
The work I’ve done in the Bowles Lab has focused on the physiological effects of cannabis on sleep in healthy humans.
I have analyzed many polysomnography (PSG) files from our sleeping test subjects, poring over recordings of their brain’s electrical activity, counting individual instances of waveforms known as sleep spindles, measuring delta power and comparing data between groups of participants and across nights. I’ve also collected data on heart rate variability, and conveyed all this information to my supervising postdoctoral scholar and my principal investigator for further analysis.
This has involved reviewing many, many squiggles (COUGH COUGH) – I mean waveforms :).
The data collected through the full monitoring system most commonly used in the Bowles Lab covers much more physiological ground, but my focus started with analysis of some of the many waveforms produced by the human brain during baseline sleep and then during sleep after consuming a small amount of dronabinol (two of three synthetic cannabis-based substances approved by the FDA).
LEARN MORE: Polysomnography
LEARN MORE: Sleep Spindles: Mechanisms and Functions
LEARN MORE: Form and Function of Sleep Spindles across the Lifespan
LEARN MORE: Sleep Quality and Electroencephalogram Delta Power
LEARN MORE: Acute effect of vaporized Cannabis on sleep and electrocortical activity
LEARN MORE: Effects of Cannabinoid Agonists and Antagonists on Sleep and Breathing in Sprague-Dawley Rats
Cannabis use has been shown to have an impact on sleep architecture (a sleep science term for the amount of time spent in each sleep stage and measures of the hallmark features of those sleep stages), and there is not conclusive evidence to indicate who would benefit from using cannabis for sleep issues and who would not benefit from using cannabis for sleep issues.
Research also suggests differences between the effects of THC (𝝙9-tetrahydrocannabinol, the primary cannabinoid in modern cannabis, though historically more balanced with cannabidiol aka CBD) for those who are new to consuming cannabis and those consuming cannabis frequently.
In cannabis-naive individuals, cannabis consumption decreases sleep latency (the amount of time it takes to fall asleep), while in those who consume cannabis frequently, it increases sleep latency (Bowles et al, 2017). Habituation (the reduction in physiological effect due to frequent repetition of stimulus) to the impacts or effects of cannabis is seen in other sleep parameters as well.
LEARN MORE: Recent legalization of cannabis use: effects on sleep, health, and workplace safety
LEARN MORE: Cannabinoid Use and Obstructive Sleep Apnea: A Retrospective Cohort Study
LEARN MORE: Molecular Pathology, Oxidative Stress, and Biomarkers in Obstructive Sleep Apnea
In the context of treating sleep disorders, the impacts of cannabis are still inconclusive.
LEARN MORE: Is There a Place for Medicinal Cannabis in Treating Patients with Sleep Disorders? What We Know so Far
Surgery

My own health journey in the treatment of sleep apnea might eventually include maxillomandibular advancement surgery, as Dr. Avram Gold himself pointed out to me when I ran into him at a poster session at SLEEP2023. It can cost $40,000-$60,000, so unless a generous surgeon offers, it’ll have to wait until my insurance recognizes my condition as chronic or I win the PowerBall.
Weight loss is often recommended as a first-line treatment for obstructive sleep apnea, but because obstructive sleep apnea can have more than one cause, the effectiveness of weight loss as a therapeutic intervention (and the ethics of weight loss as a recommendation given the many factors that can impact weight gain and prevent weight loss even in compliant patients) are not straightforward (Sutherland et al, 2016). Sometimes the issue is structural, though being told to lose weight is still the first-line treatment for obstructive sleep apnea- even if you aren’t overweight (I am). The assumption is that the weight of the throat is causing excess pressure on the airway, leading to collapse; in conditions such as mine, someone could be underweight and still suffer from obstructive sleep apnea due to the structural instability caused by faulty collagen matrices.
LEARN MORE: Is maxillomandibular advancement an effective treatment for obstructive sleep apnea?
I have a rare disease (though its rarity is always being debated), the essence of the physiological impacts of which is the production of faulty collagen matrices. Given the pervasiveness of collagen in the body, my condition has global physiological effects.
My vascular system requires more external support than most; compression gear is helpful, but no longer sufficient to preserve the previously invisible status of my disabilities. At the beginning of Summer 2023, I became an ambulatory wheelchair user so that I could stay in school and keep working in research. It’s no wonder that people with conditions like mine frequently suffer from sleep apnea, as our airways are significantly more susceptible to collapsing than the airways of people with functional autonomic nervous systems who produce sturdy collagen matrices.
Improve your sleep!
The burden placed on the human body by untreated sleep apnea can contribute to the exacerbation of other health conditions, so sleep medicine can be preventative medicine in more ways than one.
If you find your health degrading faster than standard human aging, it makes sense to look into it; my own sleep study and subsequent sleep apnea diagnosis was prompted by cartoonish snoring- but not from me.
When I received my rare disease diagnosis, I was told to prioritize getting more sleep, which I immediately started working towards. My spouse has always been a horrifically impressive snorer, and I have always been a ridiculously light sleeper, so as I was trying to get more sleep I was keenly aware of the obstacle to my rest that my spouse’s snoring represented. I finally got frustrated enough to search “how to stop someone from snoring,” and after some reading, I urged my spouse to get a sleep study done; sleep apnea and treatment with a CPAP immediately followed. From my perspective, the snoring had just been replaced by the noise of the CPAP (which is admittedly much much quieter), but I saw my spouse’s health and quality of life improve dramatically within weeks, with an improved mood being one of the first noticeable changes. Soon afterward, my spouse experienced improved cognition (likely due to neurological repairs executed after resolving the hypoxia characteristic of obstructive sleep apnea), and started to notice in me enough of the symptoms I had described witnessing to prompt me to get my own sleep study. It turns out that, though quieter, my sleep apnea was significantly more severe than my spouse’s; I’m just one case, but I hope my one case of quiet apnea prompts other quiet sleepers to investigate why they wake up tired with their healthcare provider of choice.


