Post by Allan Gaither, an undergraduate working on his Bachelor’s Degree, majoring in Psychology and minoring in Interdisciplinary Neuroscience at the Honors College of Portland State University.

While traveling school to school with NW Noggin I’ve engaged with students in a number of amazing ways, from handling brains with them to creating pipe cleaner models of neurons together! My favorite part of each trip though, by far, has been talking with the students about their questions.

We’ve had a lot of questions on topics varying from ADHD to epilepsy to traumatic brain injuries, but the one that stood out most to me was from a student at Fort Vancouver High School who asked about how OCD works in the brain. I just knew I had to look deeper into it!

So what is OCD?
OCD, or Obsessive Compulsive Disorder, is an anxiety disorder that is characterized by – you guessed it – obsessions and compulsions. But what does that actually mean?

Well, obsession is the term that is used clinically to describe the experience that someone with OCD has when their brain gets sort of stuck on an unwanted intrusive thought, image, or feeling. These can take a whole lot of energy and feel all-consuming in a person’s head. Obsessions take many forms but some of the more common obsessions are those that center around cleanliness and forgetfulness. “Did I turn off the oven?” “Is my food unclean and unsafe to eat?”
But obsessions also target less easy to talk about topics as well.
“What if that person wants to hurt me?” “What if I want to hurt that person??” “Oh no!” This might sound kind of scary, but it’s important to understand that these thoughts are intrusive and harmful only because the person having them is distressed by them!
In OCD, a person’s intrusive thoughts do not represent repressed desires or secret wishes, they’re just the brain getting stuck on something that is upsetting to think about.
“…research has shown that most people have unwanted intrusive thoughts from time to time, but in the context of OCD, these intrusive thoughts come frequently and trigger extreme anxiety, fear, and/or disgust that gets in the way of day-to-day functioning.” –International OCD Foundation, 2025
People with OCD tend to cope with their obsessions through compulsive behaviors that often, in some way, briefly relieve the emotional weight of the obsession.
For example, someone who is obsessed with the idea that they might have left the stove on may act out the compulsion of going to check one more time, even if logically they know that the stove is off because this is the third time they’ve checked. However, acting out the compulsions brings brief relief.

LEARN MORE: About the International OCD Foundation
LEARN MORE: When Unwanted Thoughts Intrude (NIH)
LEARN MORE: Obsessive-Compulsive Disorder (OCD)
LEARN MORE: Obsessive–compulsive disorder
LEARN MORE: How to Take the Power Back from Intrusive Thought OCD
How is the brain involved?
There are a few different parts of the brain that OCD is associated with. Hyperactivity has been observed in the brains of some people who have OCD in the following areas.
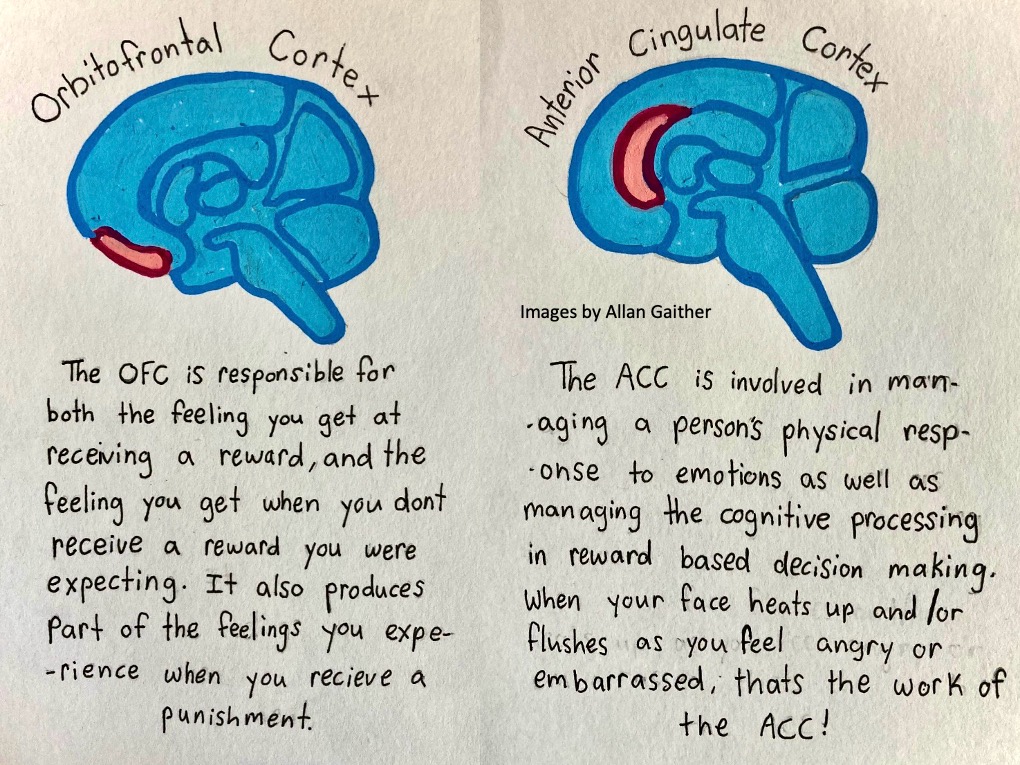
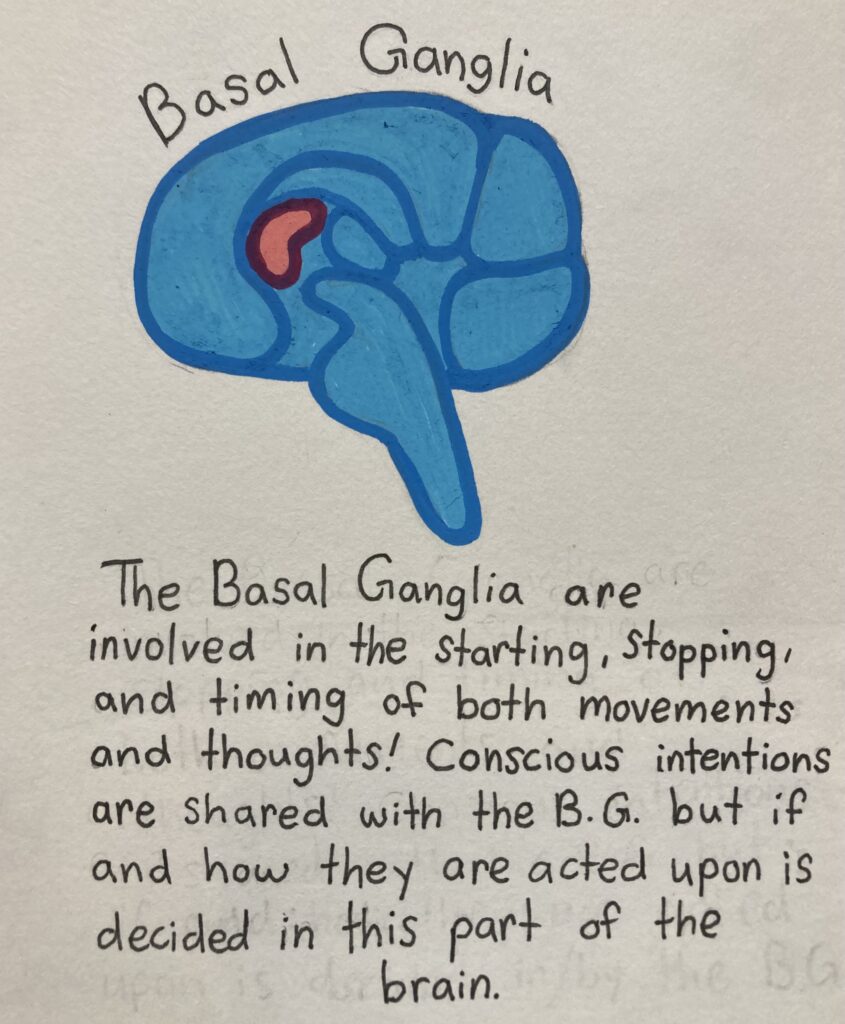

It has been observed that there is more activity and communication happening in these areas of the brain in someone who has untreated OCD when compared to someone who does not have OCD.
The trouble right now is that we’re not sure if these structures are overactive in people who have OCD in a way that is causing the disorder or if these structures have been altered as a result of the disorder, but with any luck and continued research funding we may soon find out.
LEARN MORE: The orbitofrontal cortex: reward, emotion and depression
LEARN MORE: Abnormally high degree connectivity of the orbitofrontal cortex in OCD
LEARN MORE: The cingulate cortex and limbic systems for emotion, action, and memory
LEARN MORE: Neuroanatomy of the Cingulate Cortex
LEARN MORE: Overactive action monitoring in obsessive-compulsive disorder
LEARN MORE: The Neural Signatures of Shame, Embarrassment, and Guilt
LEARN MORE: What Causes OCD?
How is OCD treated?
Now that we have a grasp on what OCD is and on the related functions of some of the brain structures thought to be involved, I’m sure the question has occurred to you: What are the treatments?
Fortunately there are several different treatment options available for OCD.
Psychotherapy
Cognitive Behavioral Therapy (CBT) is highly recommended in combination with Exposure and Response Prevention (ERP) therapy to treat OCD. In a session of ERP a person who has OCD works with a therapist on confronting and experiencing their intrusive thoughts, fears and obsessions while the therapist helps them sit through the experience without acting out their compulsions, teaching them different, healthier ways to experience the distress.



LEARN MORE: Cognitive–Behavioral Treatment of Obsessive–Compulsive Disorder
LEARN MORE: Cognitive-Behavioral Therapy for Obsessive-Compulsive Disorder
LEARN MORE: Efficacy of cognitive-behavioral therapy for obsessive-compulsive disorder
Medications
One of the medicinal approaches to OCD is the use of Selective Serotonin Reuptake Inhibitors, or SSRIs. These are a type of medication usually used to treat depression and anxiety and they work by gradually increasing the amount of serotonin in the brain by preventing it from being cleared from the synaptic gaps between neurons. SSRIs approved for use in treating OCD include Prozac, Luvox, and Zoloft, though there are others.
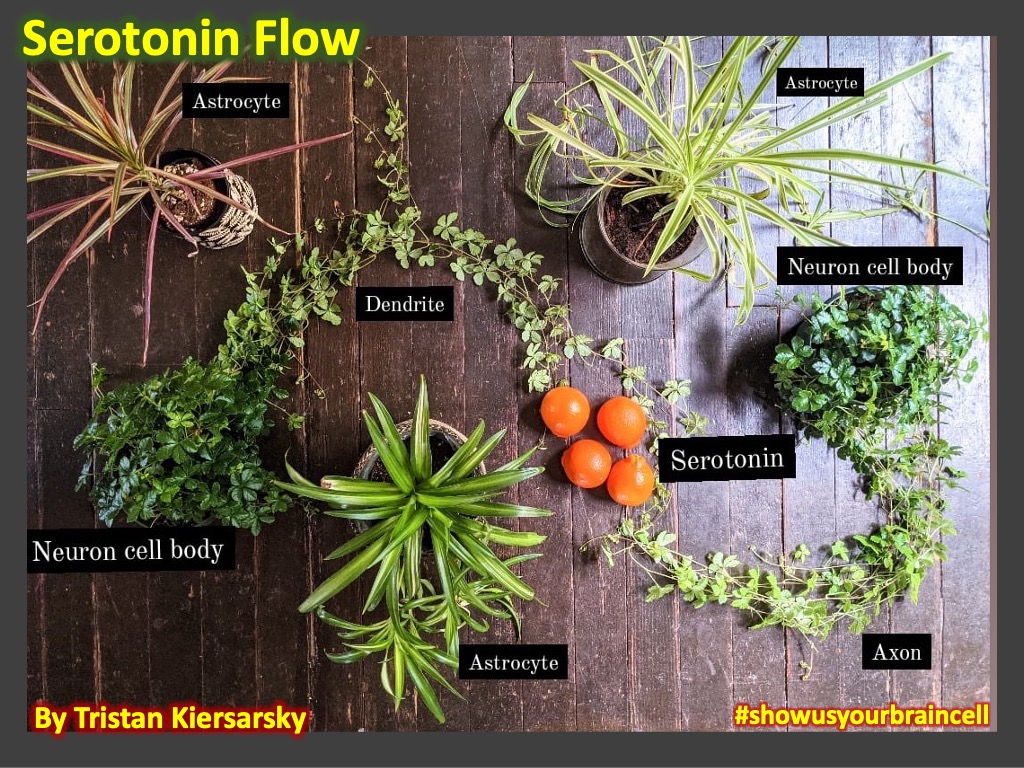
LEARN MORE: Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for OCD
LEARN MORE: Sertraline and fluoxetine treatment of obsessive-compulsive disorder
LEARN MORE: Moving beyond first-line treatment options for OCD
If SSRIs aren’t quite working, and ERP is already in practice, the next step is to add antipsychotic medication. Aripiprazole, Risperidone, and Haloperidol are the antipsychotics recommended in treatment of OCD. Ideally a patient will be utilizing ERP as well as medication if ERP alone is not generating improvements as the combination of psychotherapy and medication is thought to be most effective.
LEARN MORE: The Role of Antipsychotics in OCD
LEARN MORE: Pharmacotherapy for Treatment-Resistant Obsessive-Compulsive Disorder
Additional approaches
In some cases OCD can be quite treatment resistant and there are other tools that can be used if medicine and therapy isn’t cutting it. The Mayo Clinic mentions that Deep Brain Stimulation (DBS) as well as Transcranial Magnetic Stimulation (TMS) are also used in cases of very treatment resistant OCD.
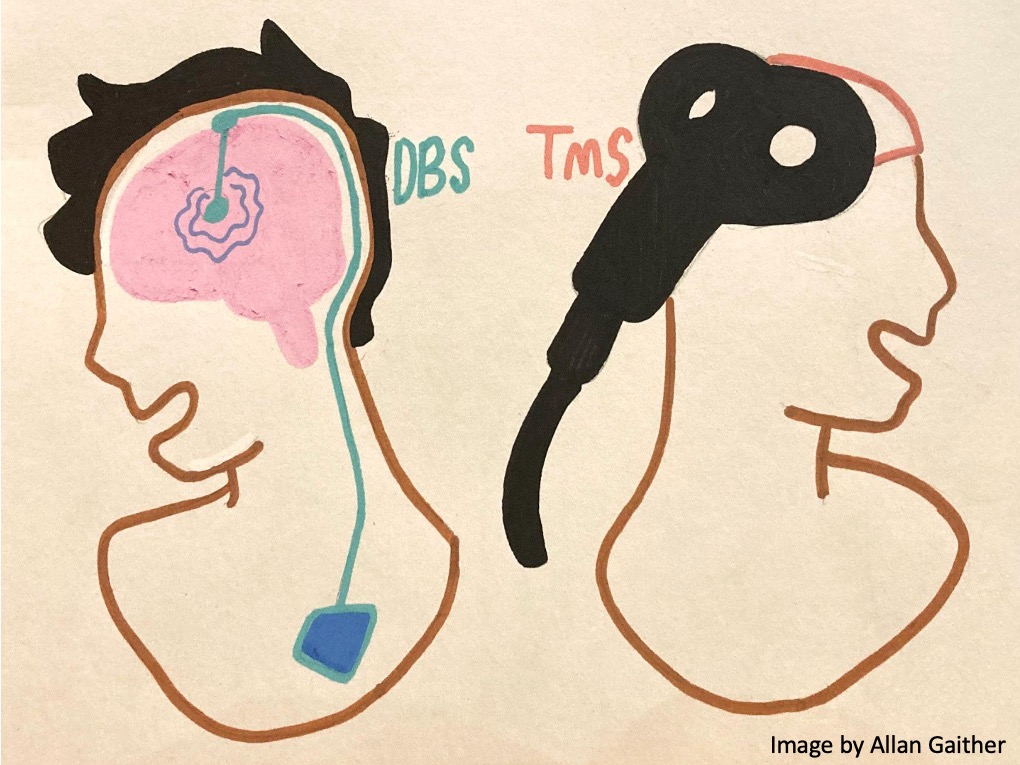
The clinic explains that in DBS, electrodes are implanted in certain parts of the brain and that the electric stimulus helps manage impulses that aren’t typical. It is also mentioned that DBS is not very commonly used. TMS is described as less intrusive and non-surgical and involves sessions where a patient has magnetic fields used to stimulate nerve cells in the brain in order to ease symptoms of OCD.
LEARN MORE: Transcranial magnetic stimulation in obsessive-compulsive disorder
LEARN MORE: Deep brain stimulation for obsessive-compulsive disorder
LEARN MORE: Obsessive-Compulsive Disorder (Mayo Clinic)
LEARN MORE: Treatment – Obsessive compulsive disorder (OCD)
Outreach with Northwest Noggin has been an incredible experience.

It has been very cool to engage with the curiosity of elementary, middle, and high school students across Portland, Vancouver, and Astoria. I am glad to have had the opportunity to study and talk with students about OCD and other mental health conditions while traveling school to school!

Stay Curious!


