Post by Becky Martinez, undergraduate in Psychology pursuing a minor in Interdisciplinary Neuroscience at Portland State University. Becky is currently an undergraduate research assistant at the Advancing Research in Pediatric Pain (ARPP) Lab at Oregon Health and Sciences University.

Time for a story!
When 14-year-old Ralphie is playing football, he is tackled and breaks his arm.
LEARN MORE: Youth Football Injuries: A Prospective Cohort
LEARN MORE: Sports-Related Injuries in Adolescent Athletes: A Systematic Review
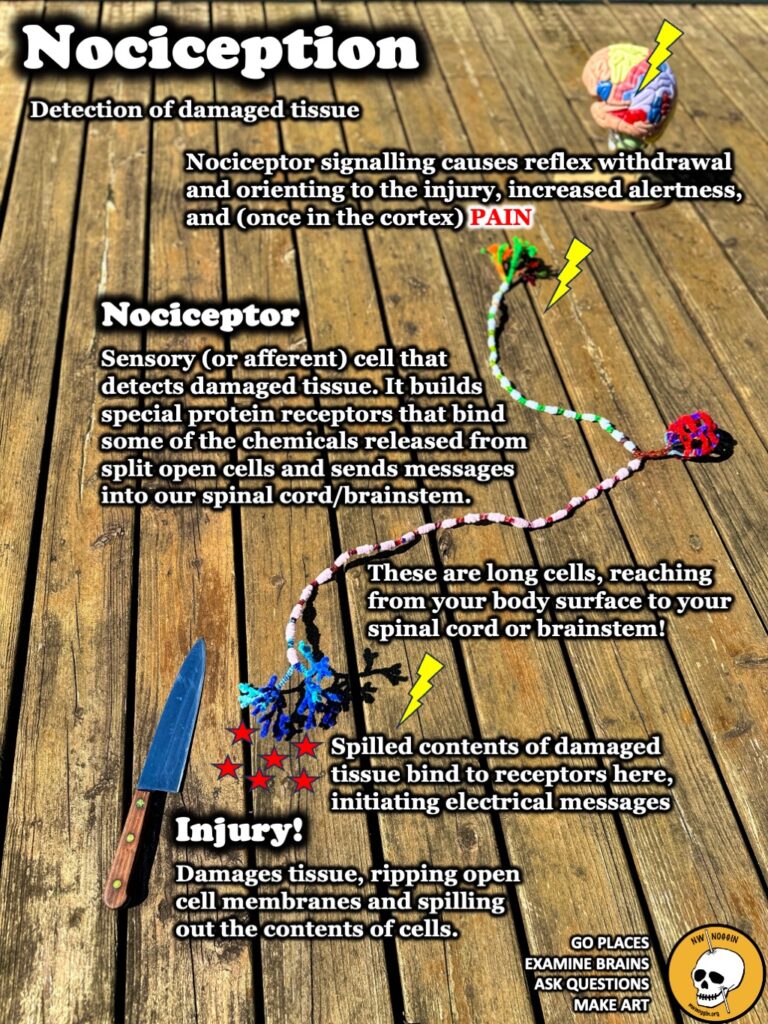
When the break occurs, Ralphie’s neurons send signals to his brain through his spinal cord. Neurons that detect injury are called nociceptors, and they are like long wires that carry electrical messages of bodily damage. Nociceptors identify injury by sensing the chemicals released from damaged cells.
His brain interprets the signals as pain which communicates to Ralphie that he needs help.
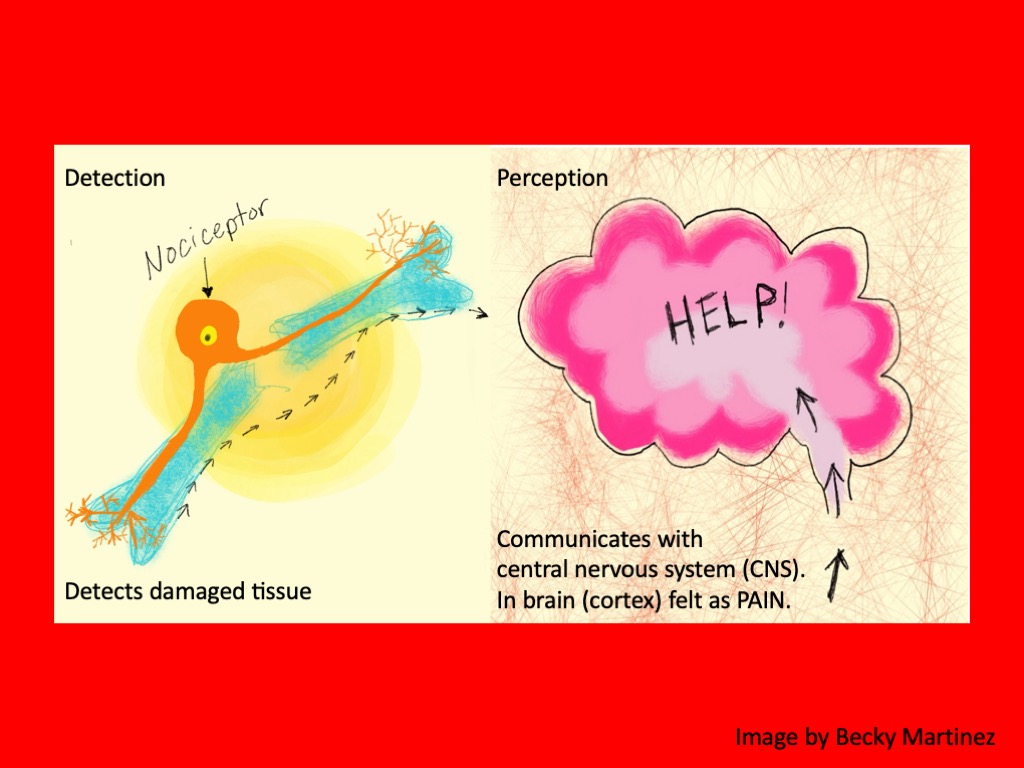
LEARN MORE: Nociceptors: the sensors of the pain pathway
LEARN MORE: General Pathways of Pain Sensation and Major Neurotransmitters Involved in Regulation
LEARN MORE: A Brain on Opioids
His parents take him to the hospital as quickly as they can. During the trip to the hospital, Ralphie’s brain releases natural painkillers called endorphins that are the perfect fit to activate special proteins embedded in his neurons called opioid receptors.

IMAGE SOURCE: What are Opioids & Opioid Addiction?
Release of endorphins (and other “endogenous” (or “made by the body”) opioids) is part of the normal activation of the brain’s dopamine reward system. As a result of ongoing research, scientists now know that more neurotransmitter systems are involved in our experience of motivation and reward than dopamine alone, including glutamate (an excitatory transmitter) – and opioids.

IMAGE SOURCE: The molecular neurobiology and neuropathology of opioid use disorder
LEARN MORE: Understanding Endorphins and Their Importance in Pain Management
LEARN MORE: Roles of β-Endorphin in Stress, Behavior, Neuroinflammation, and Brain Energy Metabolism
The opioid system in our brains plays a crucial role in reinforcing specific behaviors, which means it affects how rewarding or motivating certain activities or substances feel. Over years of research, it’s been found that different parts of this system can either increase or decrease the likelihood of us seeking out specific rewarding experiences.
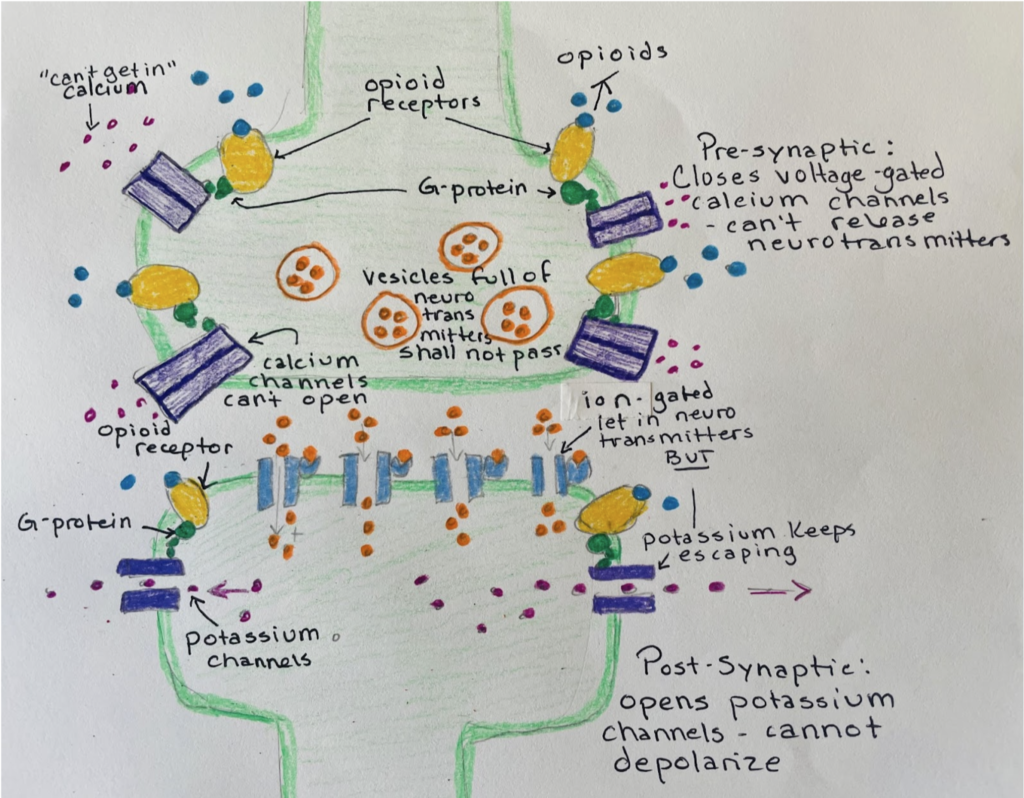
IMAGE SOURCE: Fentanyl On The Brain, by Rebecca Chevrel at Portland State University
Opioid action at opioid receptors reduces the ability of our nociceptors to send those unpleasant messages of injury to the brain – making Ralphie feel a little better. But this is only temporary pain relief that lets him remain calmer until he receives the help he needs.
After the doctors and nurses help Ralphie and time passes, Ralphie experiences lingering pain and anxiety, so the doctor prescribes Ralphie some opioid painkillers after his arm is set.

Opioid painkillers are so chemically similar to our own endorphins that they fit the exact same way as our naturally made endorphins fit on the opioid receptor – this stops the pain signals. Ralphie feels relief. Unfortunately, that relief is also temporary.

IMAGE SOURCE: What are Opioids & Opioid Addiction?
If Ralphie does not have enough protective factors – like using ibuprofen instead of too many opioids, and friends who don’t use illegal drugs, he may become dependent on opioids. Addiction to opioids (now called an opioid use disorder) comes with a whole host of negative consequences.
LEARN MORE: Opioid use disorder
LEARN MORE: Research on protective factors
LEARN MORE: Negative stress and childhood pain
LEARN MORE: Risk and Protective Factors Associated With Drug Use Among Youth
Here’s what’s happening in Ralphie’s brain as he continues to take opioids
The ventral tegmental area (or VTA) in the brain influences a lot of behaviors, including reward processing, aversion, stress modulation, drug addiction, learning and memory! Within the VTA, there are neurons that release the neurotransmitter dopamine. These dopamine neurons receive inputs from other cells that release an inhibitory neurotransmitter called GABA, which usually acts to calm them down.

IMAGE SOURCE: Princeton researchers peek into deepest recesses of human brain
LEARN MORE: Input-specific control of reward and aversion in the ventral tegmental area
LEARN MORE: VTA GABA Neurons at the Interface of Stress and Reward
Dopamine feels good and so your brain seeks more – it may find it from cookies, hugs, or even drugs. Dopamine is released when we want something – this anticipation is motivating, making us eager to keep going. When we get a reward for the first time, like the taste of a delicious cookie, our VTA releases even more dopamine. For future cookies dopamine is released mostly when we detect stimuli (for example, the person who gave us that first cookie) that predict more reward if we do something.
This is a cycle of motivation, reward, and reinforcement.
The GABA neurons are special inhibitory cells that act like crosswalk guards for dopamine. They slow down its release until something especially nice, novel or exciting happens. These neurons also have opioid receptors, which help them do their job of controlling dopamine.
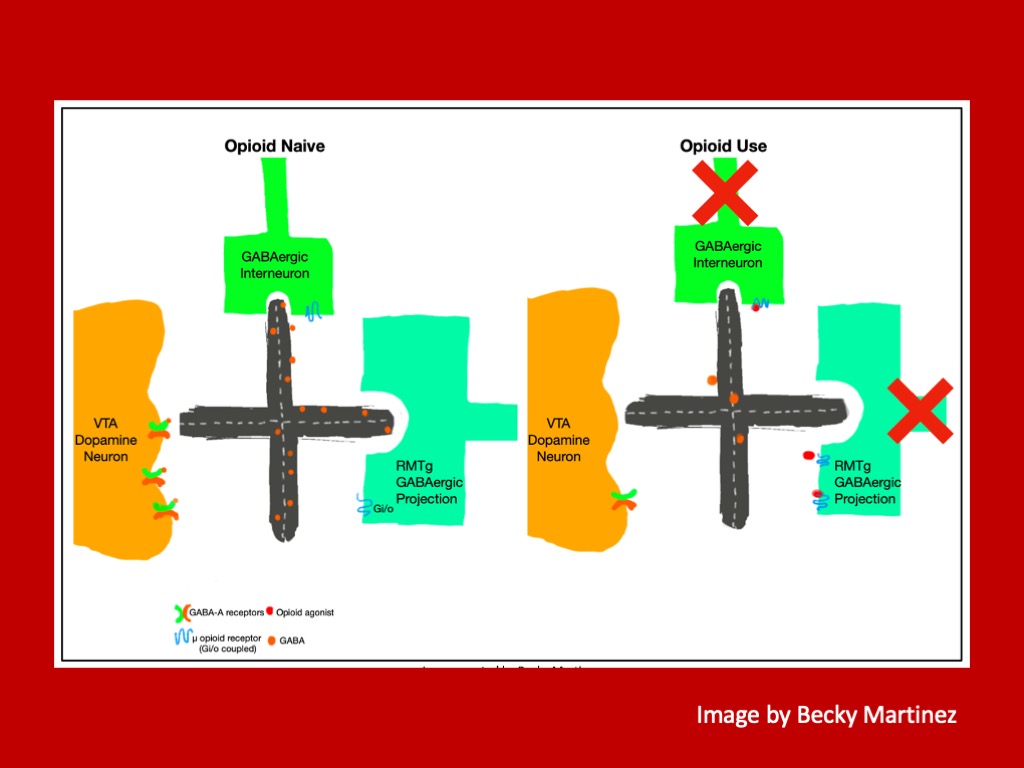
When Ralphie takes the opioid painkiller prescribed by the doctor, these drugs unlock the opioid receptors which turns off the inhibitory GABAergic neurons – which is like the crosswalk guard going on a lunch break. With nothing to slow down the dopamine, it can flood in.
The rush of dopamine feels motivating to Ralphie – but only for a short time.
Everyone’s brain attempts to protect them by trying to maintain homeostasis – which means your body wants to reach a point of stability. To try to get balanced, Ralphie’s inhibitory neurons start working overtime – even though the opioid receptors are being activated by the painkillers.
This means it is harder and harder for Ralphie’s brain to release dopamine the longer he takes the painkillers. This could lead Ralphie to take more and more of the painkillers to have the same effect they did when Ralphie first started taking them. This is called building a tolerance. When Ralphie runs out of opioid painkillers, those inhibitory neurons are still working extra hard and are clamping down on the dopamine neurons – making Ralphie feel awful.

LEARN MORE: Opioid Tolerance Development: A Pharmacokinetic/Pharmacodynamic Perspective
Ralphie may experience withdrawal symptoms when he stops taking the opioids, which are deeply unpleasant. Those symptoms include nausea, cold sweats, anxiety, irritability, aches and pains.
LEARN MORE: Opiate and opioid withdrawal
The good news is that opioids are not the only source of pain relief and if Ralphie has the right protective factors, the likelihood of an opioid use disorder is reduced.

He will manage his pain and heal.
LEARN MORE: Alternatives to Opioids for Managing Pain
LEARN MORE: Non-Opioid Perioperative Pain Strategies for the Clinician: A Narrative Review
LEARN MORE: Pain Management Medications
LEARN MORE: Pharmacological Methods of Pain Management: Narrative Review of Medication Use
LEARN MORE: Medical Cannabis for Chronic Nonmalignant Pain Management
LEARN MORE: A meta-analysis of exercise dosing for the treatment of chronic pain
LEARN MORE: Evidence review for exercise for chronic primary pain
Three in Ten Teenagers Experience Chronic Pain
Roughly 30% of adolescents experience chronic pain due to circumstances like:
ACUTE NOCICEPTIVE PAIN: This is the kind of pain that comes from activating nerve endings due to injury or other causes, like a stomachache or a cut.
LEARN MORE: Advances in understanding nociception and neuropathic pain
LEARN MORE: A Review of Management of Acute Pain
NEUROPATHIC PAIN: This happens when there’s damage or a problem with the nerves themselves, causing pain even without an obvious injury.
LEARN MORE: The neuropathic pain: An overview of the current treatment and future therapeutic approaches
LEARN MORE: Neuropathic pain
PSYCHO-SOCIAL-SPIRITUAL-EMOTIONAL PAIN: This type of pain is more complex and can involve feelings, thoughts and emotions, along with physical discomfort.
LEARN MORE: Psychological, emotional, spiritual and social aspects of pain
LEARN MORE: Evaluating Psychosocial Contributions to Chronic Pain Outcomes

While in Ralphie’s fictional case his ongoing pain stemmed from a sports injury, it’s more common for a young person’s chronic pain to involve a combination of these factors.
Treating Pain
The Comfort Ability Program is designed to support children, parents, and caregivers in effectively managing recurring functional symptoms such as chronic pain (including nerve, muscle, or joint pain, headaches, abdominal pain, etc.), nausea, dizziness, fatigue, and muscle weakness.
Through this program, participants gain insights into the workings of the nervous system and how psychological strategies can play a vital role in symptom management. It equips individuals with a range of evidence-based coping skills rooted in cognitive behavioral therapy, empowering them to better navigate their symptoms.
Delivered through workshops, health chats, newsletters, and various other resources, the Comfort Ability Program caters to teens and parents/caregivers alike. These workshops are held across the United States, Canada and Australia, providing widespread accessibility to its effective offerings.
Here are additional resources for youth experiencing chronic pain:
LEARN MORE: The Comfort Ability® Program
LEARN MORE: Advancing Research in Pediatric Pain Lab Resources
LEARN MORE: Cassie + Friends Resources
LEARN MORE: Creative Healing for Youth in Pain (CHYP)
My Work for the ROAM Project at OHSU
I’m pleased to have joined the Advancing Research in Pediatric Pain (ARPP) Lab at OHSU, led by Drs. Anna Wilson and Amy Holley. Our lab focuses on understanding and alleviating chronic pain in children and adolescents. Their interdisciplinary research examines the interplay of chronic pain, parenting, and psychological factors to identify prevention strategies and improve treatment outcomes.

LEARN MORE: Advancing Research in Pediatric Pain Lab
One prominent project that I have acted as a research assistant on is the Research of Adolescent Management of Pain (or ROAM) study. It investigates how acute injuries or pain impact teenagers and their families. Participants, aged 14-18, who have experienced recent acute pain or surgery, along with a willing parent or guardian, are invited to complete online questionnaires and brief phone interviews every six months over two years. The study aims to enhance knowledge of pain and its management in teens and offers compensation to participants.
How do I contribute to the lab as a research assistant?
As a research assistant in the ARPP lab, I’ve made several contributions to ongoing research projects. One notable contribution involved creating and presenting a scientific research poster based on data from the ROAM project, which focuses on understanding how acute pain affects teenagers and their families. This poster highlighted key findings and insights gleaned from the study, potentially contributing to the dissemination of helpful knowledge within the scientific community.

Additionally, I am conducting “timeline follow-back” phone surveys as part of our research efforts.
These surveys involve following up with both parents and children to gather detailed information about their experiences with pain, opioids and other pain-relieving substances. By conducting these surveys, I help collect valuable data that contributes to our understanding of pain management strategies and their impact on adolescents and their families.
I am currently working on a literature review to explore existing research on the impact of discordance between mother and child reported pain. In simpler terms, discordance means things aren’t quite fitting together or matching up the way they should. It’s like puzzle pieces not properly connecting, causing confusion or disagreement. My literature review will involve synthesizing findings from various studies to identify gaps in knowledge and potential avenues for future research.
By doing a literature review, I am contributing to the development of a more comprehensive understanding of how parent-child interactions influence pain experiences and outcomes.
What I’ve learned
As a research assistant in the ARPP lab, I’ve been immersed in understanding pain management complexities, especially in adolescents like Ralphie. Ralphie’s narrative underscores the nature of pain treatment, highlighting the risks associated with opioid use. Through projects like the ROAM study and conducting surveys on pain management strategies, I’ve gained insight into how acute pain impacts teenagers and families, and the importance of holistic approaches to pain management.
By expanding our knowledge of pain mechanisms, treatment modalities and risk factors, we refine approaches to mitigate potential harms associated with opioids. From opioids to therapy, ibuprofen and cannabinoids, it’s essential to weigh efficacy, safety, and individual patient factors.
LEARN MORE: Cognitive-behavioral therapy for patients with chronic pain
LEARN MORE: Integrated cognitive behavioral therapy for chronic pain
LEARN MORE: An Overview of Clinical Pharmacology of Ibuprofen
LEARN MORE: PharmGKB summary: ibuprofen pathways
LEARN MORE: Medical Cannabis for Chronic Nonmalignant Pain Management
LEARN MORE: Popping off (& pot) @ p:ear
While opioids offer potent acute relief, they also carry addiction risks.
Ibuprofen, in contrast, provides effective relief, albeit not always as potent as opioids, but with low risk of addiction. Cognitive behavioral therapy based programs including the Comfortability Workshop require committed practice, and cannabinoids show promise but require further research – especially with regards to adolescents.
I’m excited to be a part of this research. Integrating new discoveries into clinical practice ensures safer, more effective pain management interventions tailored to adolescents’ diverse needs.


