NW Noggin presented a workshop for the Washington State Psychological Association (WSPA) on Saturday, September 10 at North Seattle Community College…
A second workshop will be presented at WSU Vancouver in 2017 (date/time TBD)…
WORKSHOP SYLLABUS
WSPA Art Pain and Cannabinoids 2016
Cannabis sativa from Vienna Dioscurides, 512 AD
SLIDES FOR PART ONE
Bill Griesar, PhD.
Instructor and Outreach Coordinator, Neuroscience, WSU Vancouver
Instructor, Psychology, Portland State University
Affiliate Graduate Faculty, Behavioral Neuroscience, OHSU
Neuroscience Coordinator, nwnoggin.org
Bill-WSPA-marijuana-SLIDES-fall-2016 (ppt)
Bill-WSPA-marijuana-SLIDES-fall-2016 (pdf*)
*clearer on a mobile device
Chronic pain is a pressing concern for medicine and psychology, and available therapeutic drugs, particularly opioids, often have serious and even deadly side effects…
LEARN MORE: Why the Pain Drug That Killed Prince Can Be Especially Dangerous
Opioid use, and abuse, is astonishingly widespread in the United States…
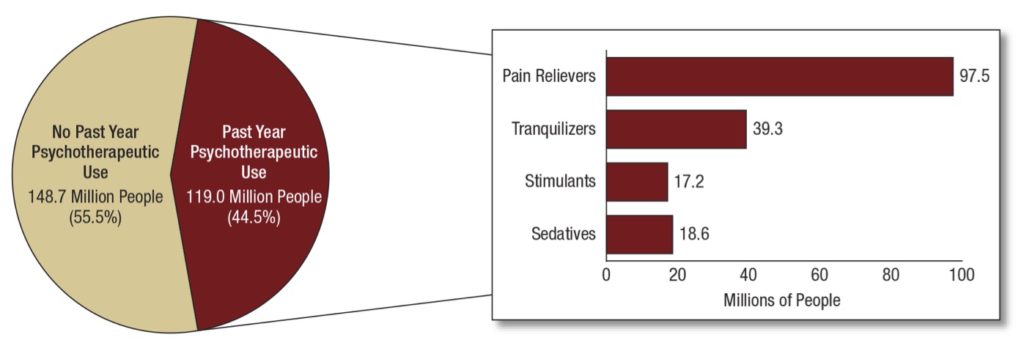
New statistics released in September 2016 by the Substance Abuse and Mental Health Services Adminstration (SAMHSA, part of U.S. Health & Human Services), from analysis of the annual National Survey on Drug Use and Health (NSDUH), revealed the shocking extent of psychotherapeutic drug use in the United States…
From the report: “In 2015, an estimated 119.0 million Americans aged 12 or older used prescription psychotherapeutic drugs (pain relievers, tranquilizers, sedatives and stimulants) in the past year, representing 44.5 percent of the population.“
Also from the report: “In 2015, 18.9 million people aged 12 or older (7.1 percent) misused prescription psychotherapeutic drugs in the past year. ”
And: “Misuse of prescription psychotherapeutic drugs is second only to marijuana as the nation’s most prevalent illicit drug use issue.”
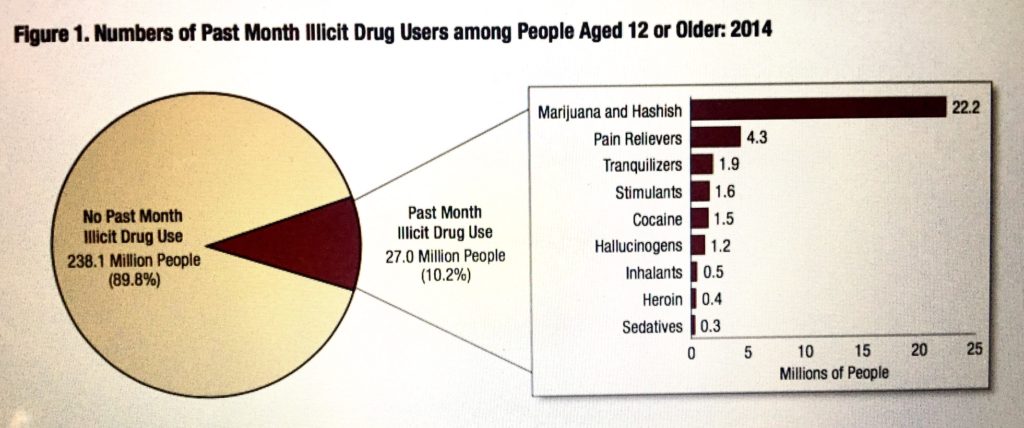
So in 2014 (from the latest statistics released by SAMHSA), 22.2 million Americans consumed marijuana, all of them lumped together as having engaged in “illicit” use – and then compared directly with the 18.9 million abusing opioids and other psychotherapeutic drugs as if these represented similar populations…
LEARN MORE: Widespread Use Of Prescription Drugs Provides Ample Supply For Abuse
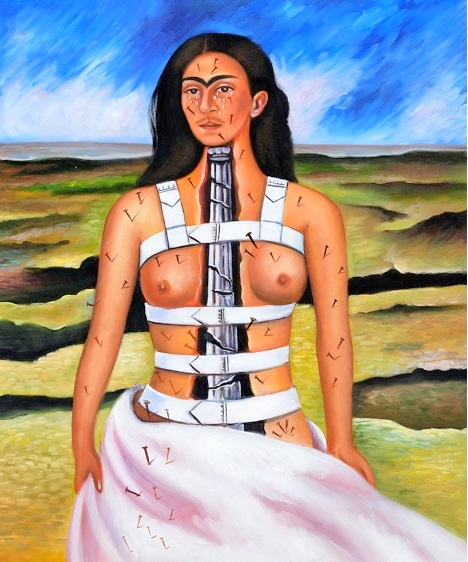
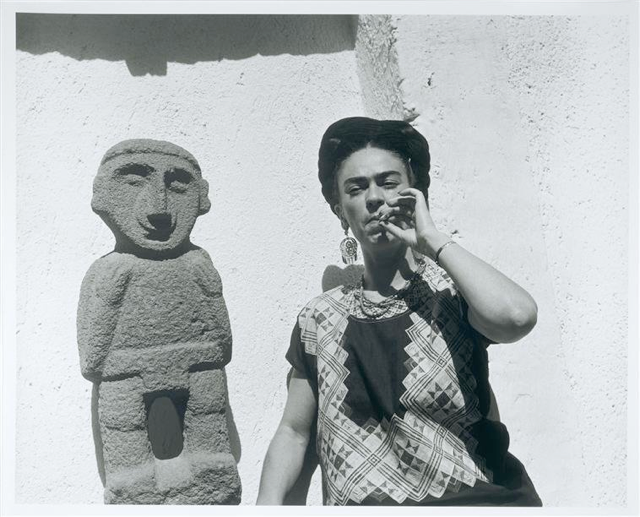
Artist Frida Kahlo survived a bus accident in 1925, which broke her spinal column, collarbone, ribs, pelvis and right leg, crushed and dislocated her right foot, dislocated her shoulder – and left her with terrible, psychologically debilitating bouts of chronic pain.
Pain impacts lives – many lives – dramatically, and the need for safe and effective treatments is clearly acute.
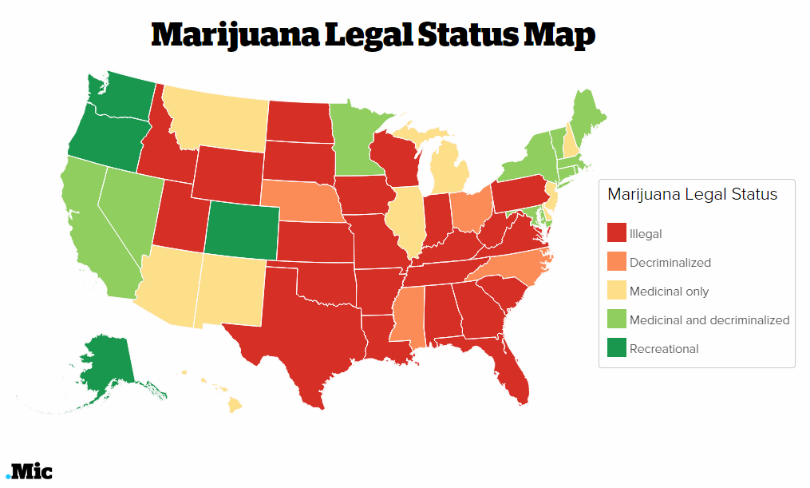
New research finds that states permitting legal access to marijuana have experienced a substantial drop in the number of opioid prescriptions…
Map source: Policy.mic
In addition, states that allow for medical marijuana, including Oregon, Washington and California, also have significantly lower state-level opioid overdose mortality rates when compared with states that prohibit legal access to cannabis for medical use…
LEARN MORE: Medical Cannabis Laws and Opioid Analgesic Overdose Mortality in the United States, 1999–2010
Legalizing marijuana cuts the number of opioid prescriptions and saves lives.
So might cannabinoids (the more than 100 psychoactive chemicals found in marijuana) effectively treat pain? One arm of the U.S. federal government (DEA) still classifies marijuana as a Schedule 1 drug, without clinical or therapeutic utility, while another (NIH) funds research suggesting the exact opposite.
Here are a few relevant research review articles (with short excerpts from abstracts) that find evidence supporting the efficacy of cannabinoids in the treatment of various forms of pain…
Cannabinoids in the management of difficult to treat pain, Ethan B Russo, Ther Clin Risk Manag. 2008 Feb; 4(1): 245–259 “Cannabinoid analgesics have generally been well tolerated in clinical trials with acceptable adverse event profiles. Their adjunctive addition to the pharmacological armamentarium for treatment of pain shows great promise.”
Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials, Lynch ME, Campbell F, Br J Clin Pharmacol. 2011 Nov;72(5):735-44 “Fifteen of the eighteen trials that met the inclusion criteria demonstrated a significant analgesic effect of cannabinoid as compared with placebo and several reported significant improvements in sleep. There were no serious adverse effects… Overall there is evidence that cannabinoids are safe and modestly effective in neuropathic pain with preliminary evidence of efficacy in fibromyalgia and rheumatoid arthritis.”
Cannabinoids as Pharmacotherapies for Neuropathic Pain: From the Bench to the Bedside, Elizabeth Rahn, Andrea G. Hohmann, Neurotherapeutics. 2009 Oct; 6(4): 713–737 “In animals, cannabinoids attenuate neuropathic nociception produced by traumatic nerve injury, disease, and toxic insults…Clinical studies largely affirm that neuropathic pain patients derive benefits from cannabinoid treatment.”
The Endocannabinoid System, Cannabinoids, and Pain, Perry G. Fine, Mark J. Rosenfeld, Rambam Maimonides Med J. 2013 Oct; 4(4): e0022 “The endocannabinoid system is involved in a host of homeostatic and physiologic functions, including modulation of pain and inflammation…phytocannabinoids in combination, especially cannabidiol and β-caryophyllene, delivered by the oral route appear to be promising candidates for the treatment of chronic pain due to their high safety and low adverse effects profiles.”
The effectiveness of cannabinoids in the management of chronic nonmalignant neuropathic pain: a systematic review, Boychuk DG et al, J Oral Facial Pain Headache. 2015 Winter;29(1):7-14 “CONCLUSION: Cannabis-based medicinal extracts used in different populations of chronic nonmalignant neuropathic pain patients may provide effective analgesia in conditions that are refractory to other treatments. Further high-quality studies are needed to assess the impact of the duration of the treatment as well as the best form of drug delivery.”
SLIDES FOR PART TWO
Jeff Leake, MFA
Instructor and Outreach Coordinator, Neuroscience, WSU Vancouver
Art Coordinator, nwnoggin.org
Leake WSPA Marijuana SLIDES 2016 (ppt)
Leake WSPA Marijuana SLIDES 2016 (pdf*)
*clearer on a mobile device
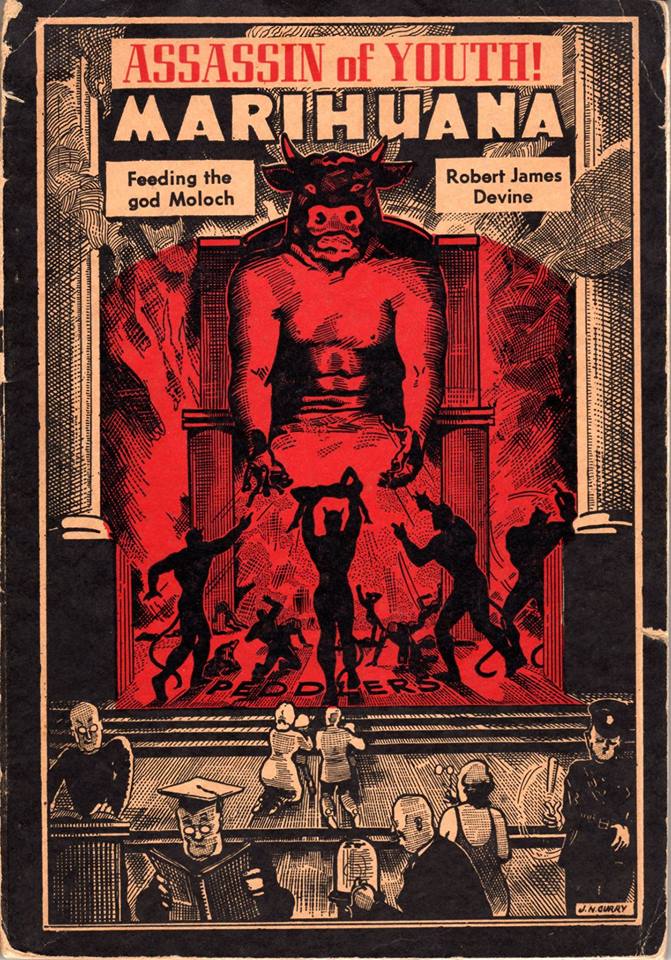
Artists have depicted (and used) cannabis for thousands of years. Examining this visual history both ancient and contemporary can tell us a great deal about what we have used cannabis for, how we have viewed it’s use, and how that has informed our current views and policies.
“How many murders, suicides, robberies, criminal assaults, holdups, burglaries and deeds of maniacal insanity it causes each year, especially among the young, can only be conjectured…No one knows, when he places a marijuana cigarette to his lips, whether he will become a joyous reveler in a musical heaven, a mad insensate, a calm philosopher, or a murderer…”
HARRY J ANSLINGER
Commissioner of the US Bureau of Narcotics 1930-1962

Fred Tomaselli, Super Plant, 1994. Psychoactive plant material, acrylic and resin on wood panel, 74 x 54″
EXPLORE MORE: Visual Culture & Cannabis With the WSPA
SLIDES FOR PART THREE
Ram Kandasamy, Graduate Student, Neuroscience, WSU Vancouver
Ram_WSPA marijuana SLIDES (ppt)
Ram_WSPA marijuana SLIDES (pdf*)
*clearer on a mobile device
Chronic pain is the most prevalent clinical phenomenon. Its disabling and distressing nature is the primary reason people seek medical attention. Despite the multitude of research surrounding the mechanisms and determinants underlying chronic pain, very few safe and effective therapies exist. The need for alternative treatments for chronic pain remains a priority.
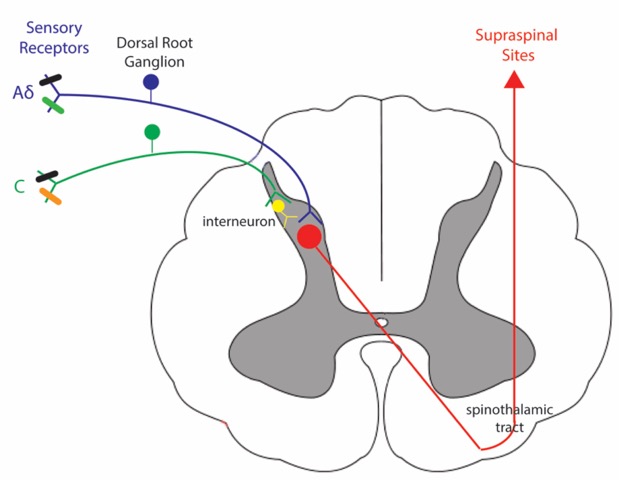
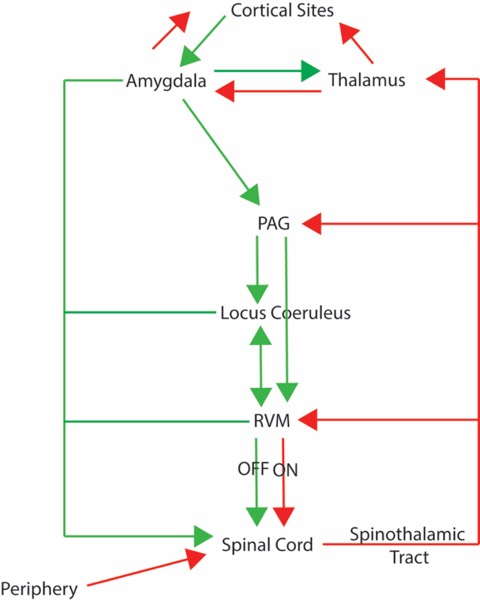
As illustrated below, pain is a complex clinical phenomenon that involves integration of multiple inputs by various regions of the central nervous system, including the brain and spinal cord. For review, see Ossipov, M. H. (2012). The perception and endogenous modulation of pain. Scientifica, 2012.
Figure 1: Ascending Pain Pathway. Aδ and C fibers have cell bodies in the dorsal root ganglion and nerve endings in the periphery. The central terminals of these fibers enter through the dorsal horn of the spinal cord and synapse onto their second order neurons. These second neurons cross and ascend to supraspinal sites along the spinothalamic tract.
Figure 2: Descending Pain Pathway. There are endogenous mechanisms that inhibit (green) and facilitate (red) pain transmission at the level of the spinal cord and via descending inhibition from cortical sites.
The use of marijuana for medicinal purposes dates back to ancient times and once held a prominent position in the United States pharmacopeia. Despite the multitude of preclinical and clinical research surrounding the pain-relieving effects of the plant, political and social factors have deemed marijuana illegal. Below is a SMALL subset of references that support the use of Cannabis and cannabinoids for the treatment of chronic pain.
Bradford, A. C., & Bradford, W. D. (2016). Medical Marijuana Laws Reduce Prescription Medication Use In Medicare Part D. Health Affairs, 35(7), 1230-1236. “…we found that the use of prescription drugs for which marijuana could serve as a clinical alternative fell significantly, once a medical marijuana law was implemented.”
Lynch, M. E., & Campbell, F. (2011). Cannabinoids for treatment of chronic non‐cancer pain; a systematic review of randomized trials. British journal of clinical pharmacology, 72(5), 735-744. “Overall there is evidence that cannabinoids are safe and modestly effective in neuropathic pain with preliminary evidence of efficacy in fibromyalgia and rheumatoid arthritis.”
Hill, K. P. (2015). Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA, 313(24), 2474-2483. “Use of marijuana for chronic pain, neuropathic pain, and spasticity due to multiple sclerosis is supported by high-quality evidence. Medical marijuana is used to treat a host of indications, a few of which have evidence to support treatment with marijuana and many that do not. Physicians should educate patients about medical marijuana to ensure that it is used appropriately and that patients will benefit from its use.”
To register for this workshop, please visit the website for the WSPA…
September 10 Workshop Series Registration