Post written by Ram Kandasamy, Neuroscience, WSU Vancouver
Ram presented his graduate research on cannabinoids and chronic pain as part of a Washington State Psychological Association workshop in September, 2016; a workshop that will also be offered at WSU Vancouver early in 2017 (date/time TBA)…
EXPLORE MORE: Art, Pain – and Pot?
The sculpture represents suffering from chronic pain. –Mark Collen
EXPLORE MORE: Pain as an art form
EXPLORE MORE: PainExhibit.org
What is pain?
Pain is defined as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”. It is important to note that pain is subjective. Pain will certainly vary from person to person. This individual variability makes chronic pain an incredibly difficult disease to treat.
Pain is protective. The best example of the protective component of pain is the acute reflex (e.g., withdrawing your hand after touching a hot stove). This reflex prevents your body from sustaining further injury and damage. In some cases, there may be prolonged pain such as swelling or bruising. This other type of protective pain allows the body to heal and repair itself.
Pain becomes a problem when it is abnormal. Abnormal pain is non-protective. That is, it plays no useful purpose. At this stage, we classify pain as a disease.
The therapeutic goal for pain researchers is to eliminate the abnormal pain without interfering with normal, protective pain.
Current treatments for pain are poor
Opioids are the most effective drugs for the treatment of pain (Portenoy et al., 2004). However, a multitude of side effects (e.g., tolerance, respiratory depression, addiction, etc.) limit their use.
When an opioid given for pain binds to its receptors, analgesia is accompanied by a wide array of side effects related to the activation of receptors involved in other functions. These include effects on the gastrointestinal tract (leading to constipation) and nervous system (leading to pupillary constriction, itch, and respiratory depression, tolerance). Furthermore, consistent opioid use may lead to a paradoxical phenomenon known as opioid-induced hyperalgesia, a condition where opioids exacerbate persistent pain.
Importantly, a large majority of pain patients report that their pain is treated poorly. As a result, developing novel treatment options for pain remains a clinical priority.
Cannabinoids provide a therapeutic avenue for the treatment of pain
Cannabis contains 537 constituents and 107 of them are unique to cannabis (i.e., cannabinoids). ∆9-tetrahydrocannabinol (THC) is a major active molecule of cannabis and has shown to be analgesic in the rat, mouse, and human.
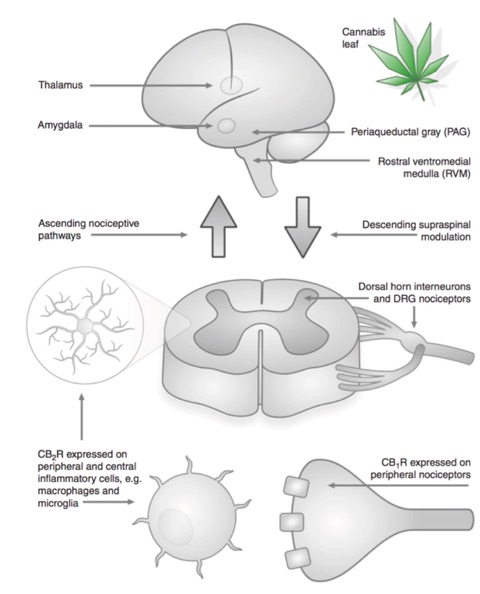
Fig. 2 (from Hosking and Zajicek, 2008)
Cannabinoid receptors are present in the pain pathway. Supraspinal cannabinoid receptors are present in areas of the brain and brainstem involved in pain transmission and perception (thalamus, amygdala, periaqueductal gray). A large density of spinal cannabinoid receptors is present in areas of the superficial dorsal horn. Cannabinoid receptors are also present in peripheral sensory nerve endings and on non-neuronal cells that participate in immune and inflammatory processes.
Very few randomized controlled trials (RCTs) have been conducted using smoked cannabis; however, a number of cannabinoid-based therapies (e.g., Nabilone, Sativex, Marinol) have been shown to be efficacious in a number of different types of pain conditions. Examples include neuropathic pain, post-herpetic neuralgia, post-operative pain, arthritis, and cancer pain. A more extensive list can be found in Russo, 2008 and Hill, 2015.
Concluding remarks
Pain impairs physical and psychological well-being. Currently available treatments, generally opioids, are not always effective and are accompanied by a number of side effects. Cannabinoid receptors are present in areas of the central and peripheral nervous system that are involved in the processing of pain. Importantly, the mechanisms underlying cannabinoid analgesia are different from any current analgesic. Therefore, cannabinoids do provide a novel treatment avenue for the treatment of pain and may have advantages compared to traditional analgesics.
References
Portenoy RK, Payne R, Passik SK. Lowinson JH, Ruz P, Millman RB, Langrod JG. Substance Abuse: A Comprehensive Textbook. 4th ed. Philadelphia: Lippincott, Williams & Wilkens; 2004. Acute and Chronic Pain; pp. 863–904.
Hill, K. P. (2015). Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. Jama, 313(24), 2474-2483.
Hosking, R. D., & Zajicek, J. P. (2008). Therapeutic potential of cannabis in pain medicine†. British journal of anaesthesia, 101(1), 59-68.
Russo, E. B. (2008). Cannabinoids in the management of difficult to treat pain. Therapeutics and Clinical Risk Management, 4(1), 245.